Articles
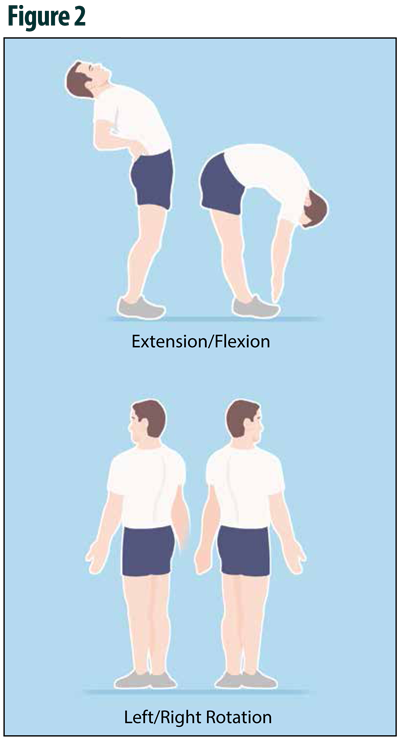
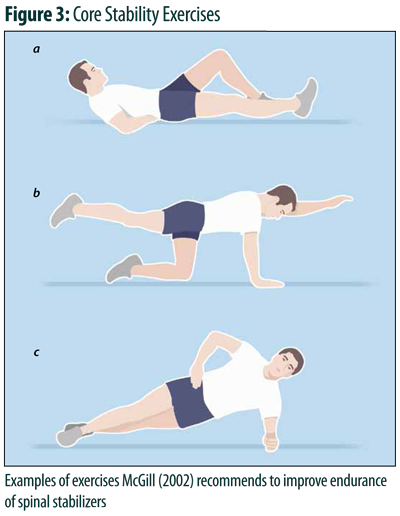
Spine and Sport: Are Athlete's Back Injuries Different?
Spine and Sport: Are Athlete's Back Injuries Different?
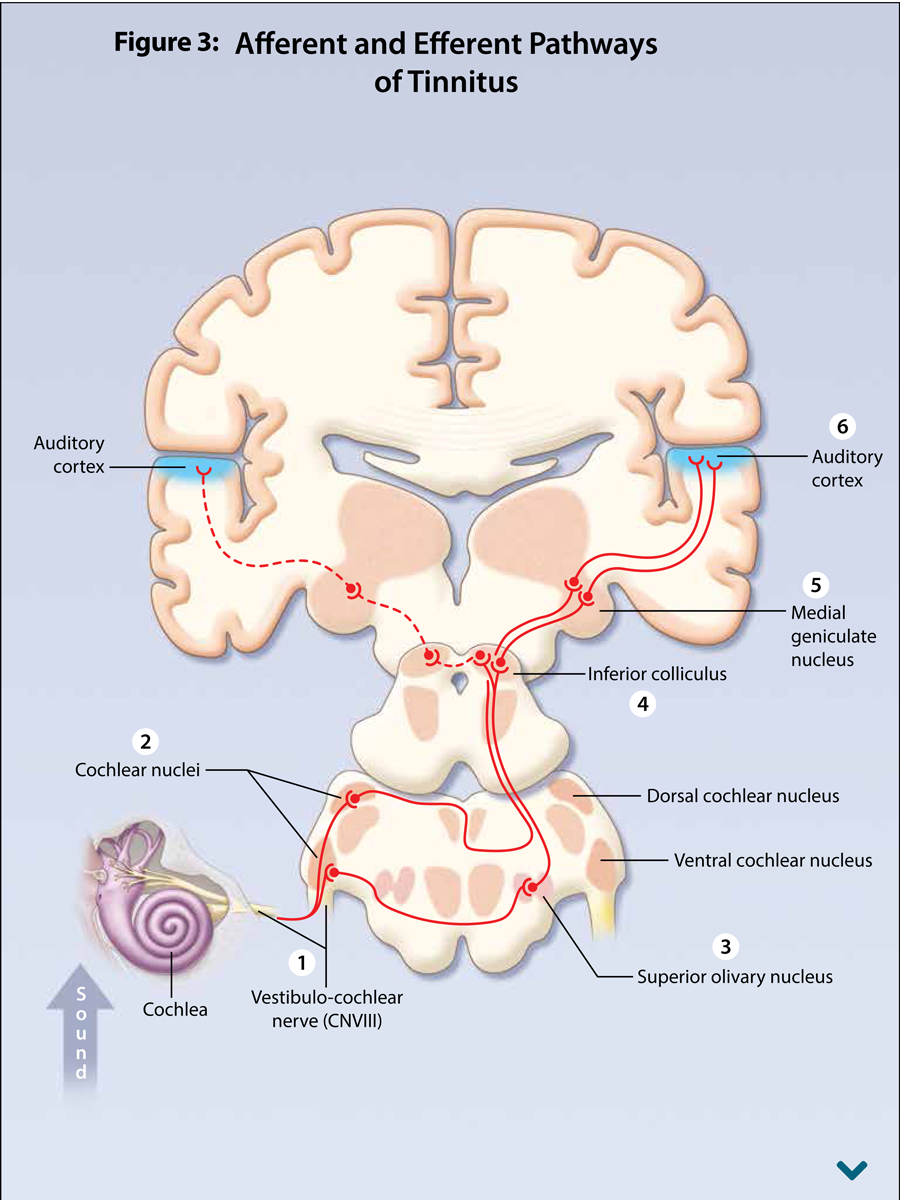
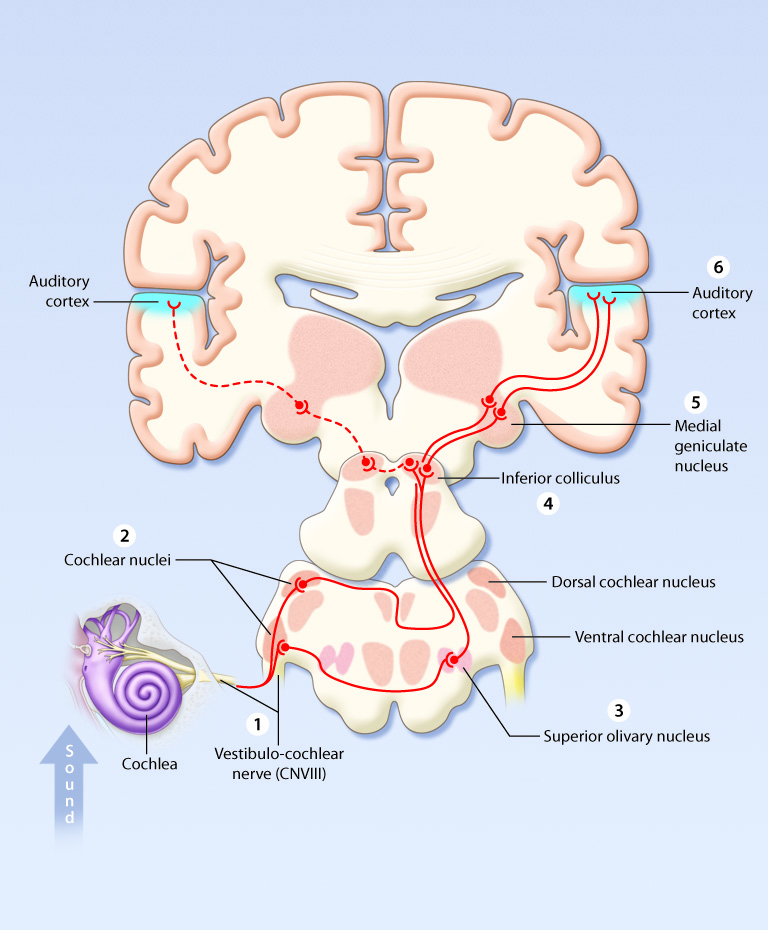
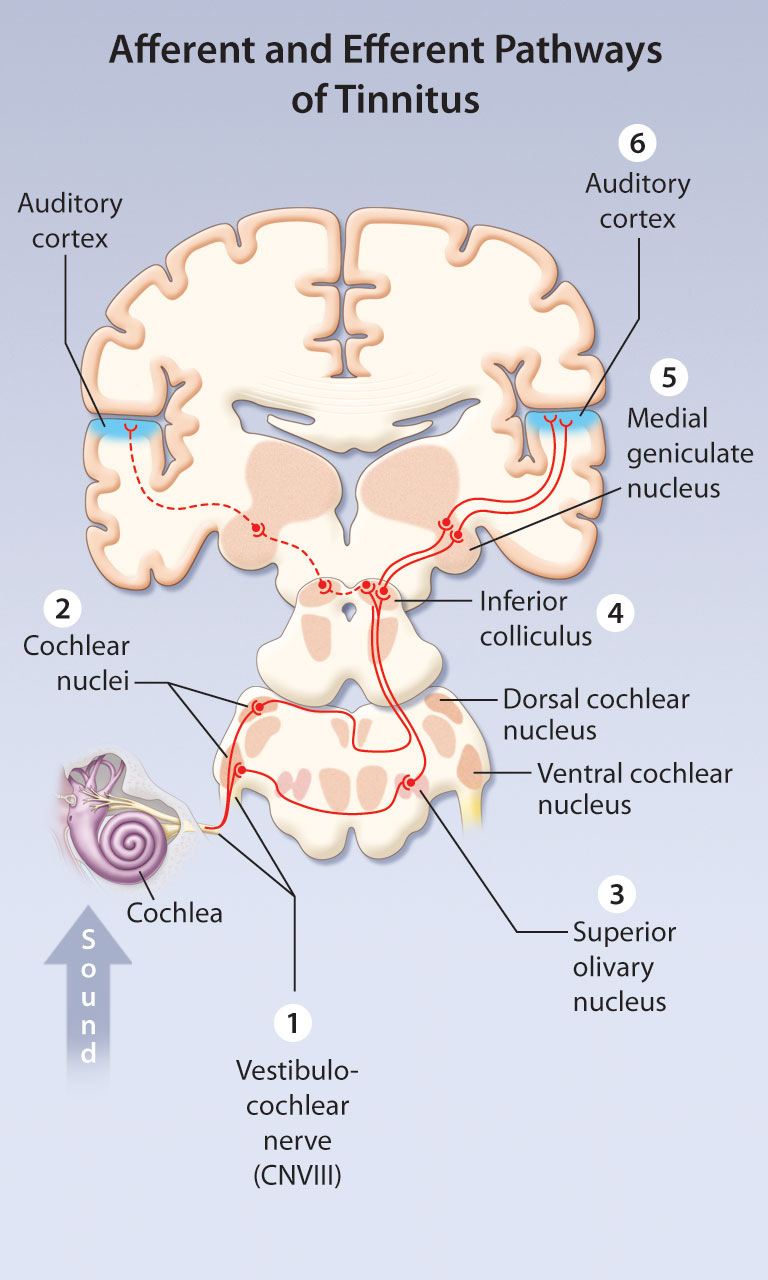
TINNITUS is an "Aura Symptom" in Need of a Multidisciplinary Approach to Facilitate Diagnosis and Treatment
TINNITUS is an "Aura Symptom" in Need of a Multidisciplinary Approach to Facilitate Diagnosis and Treatment
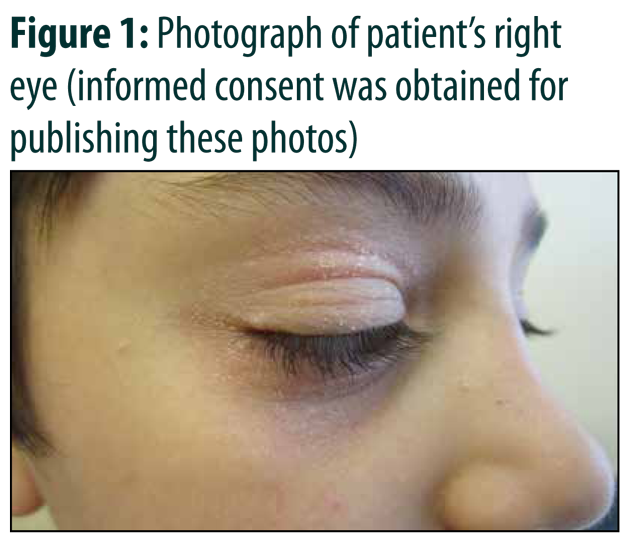
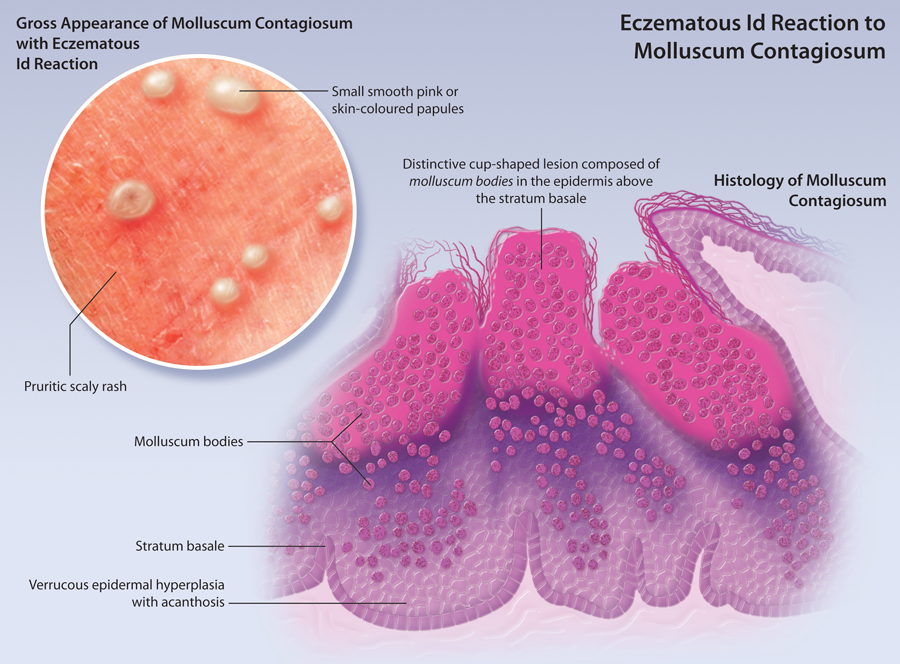
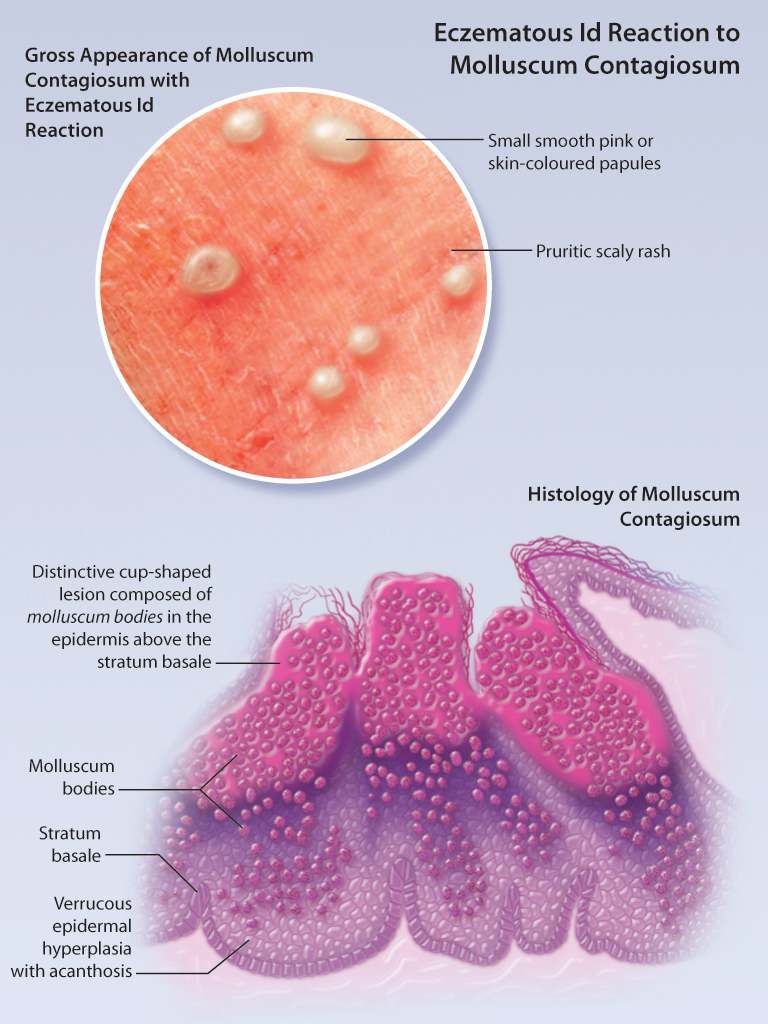
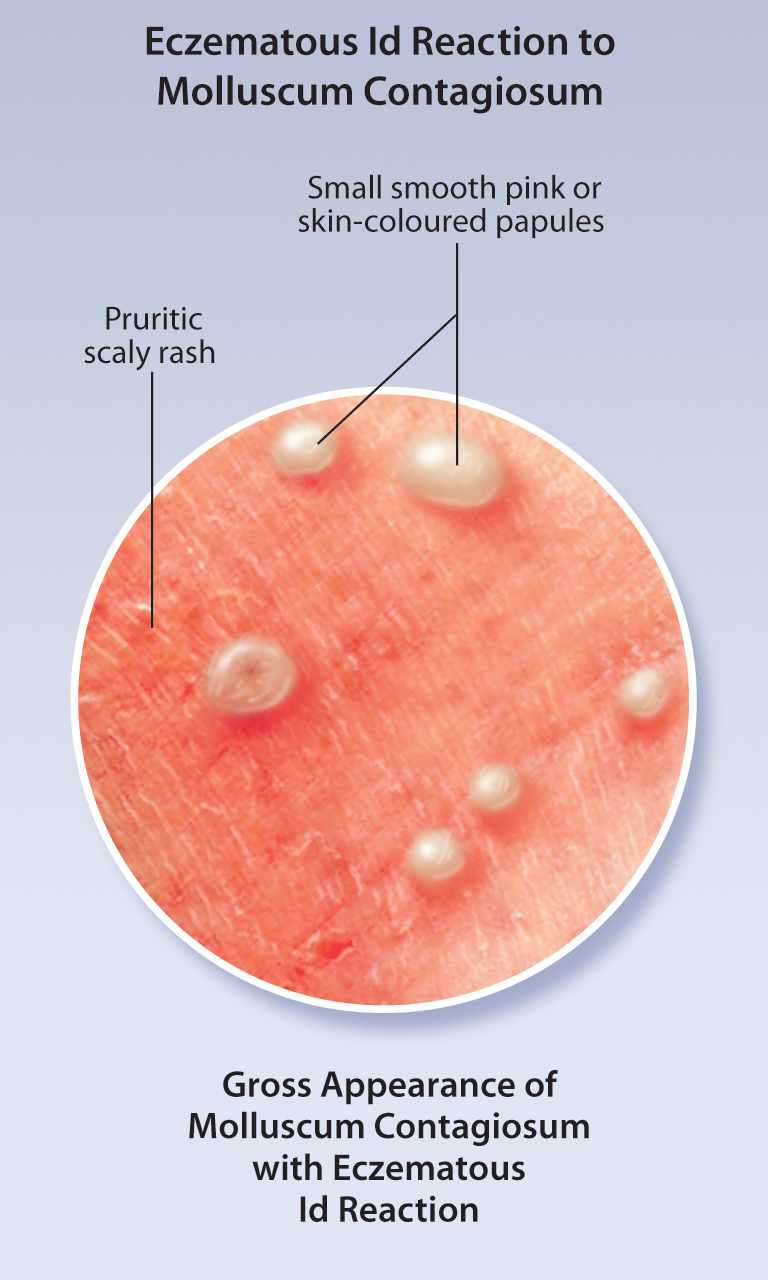
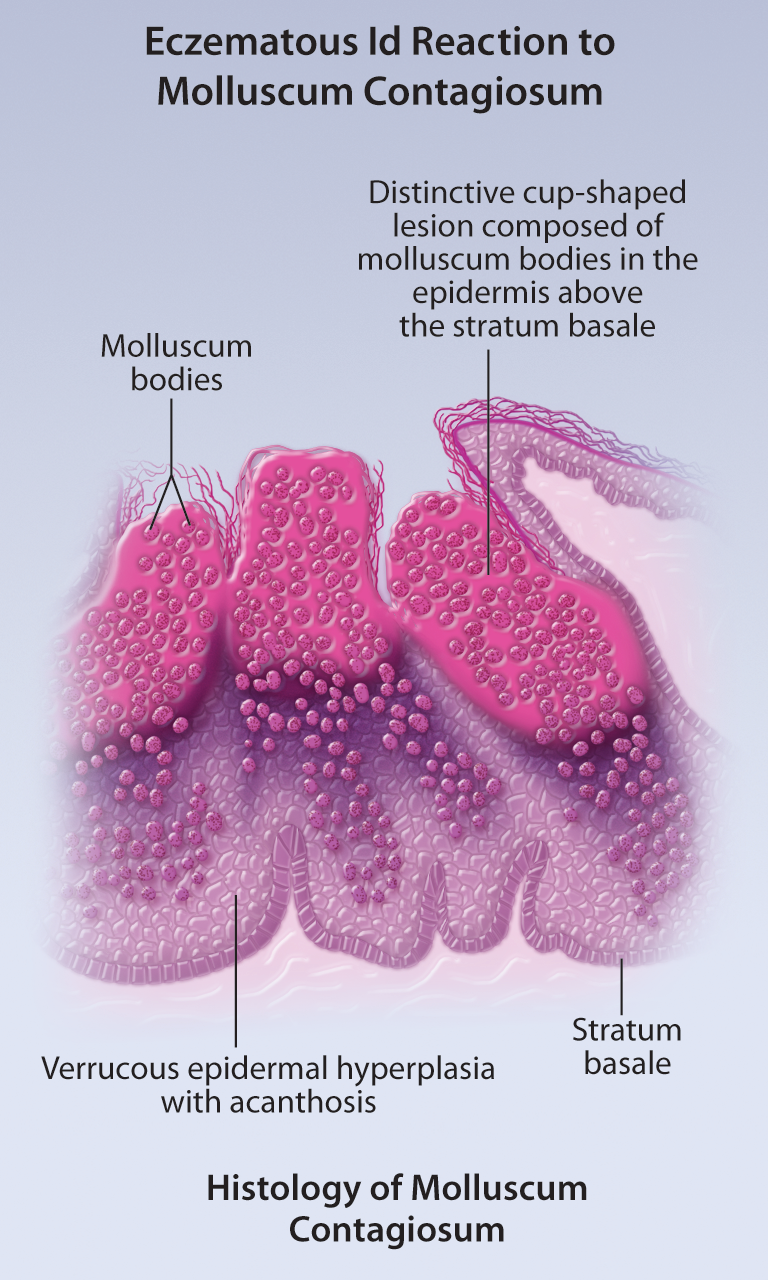
A Scaly Periorbital Rash in a Preschool-aged Boy
A Scaly Periorbital Rash in a Preschool-aged Boy
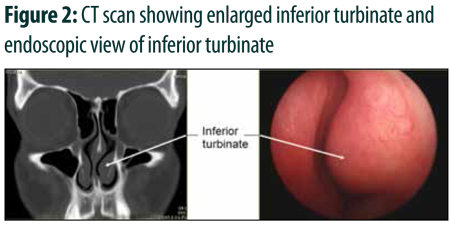
Bipolar Electrofulgration with Endoscopic Approach in Allergic Turbinates
Bipolar Electrofulgration with Endoscopic Approach in Allergic Turbinates
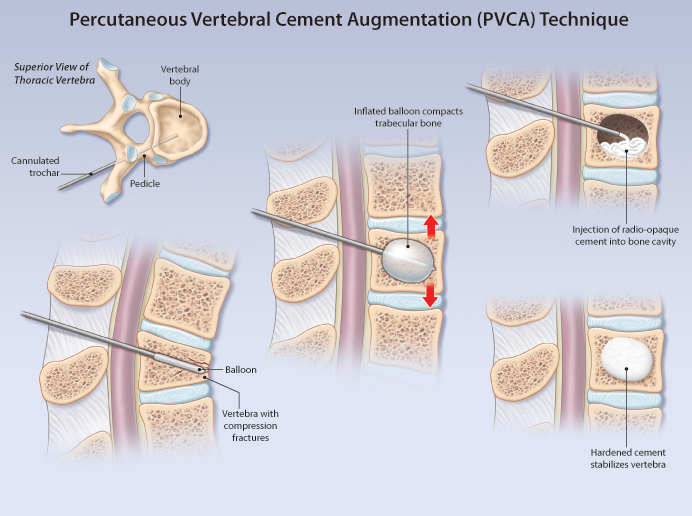
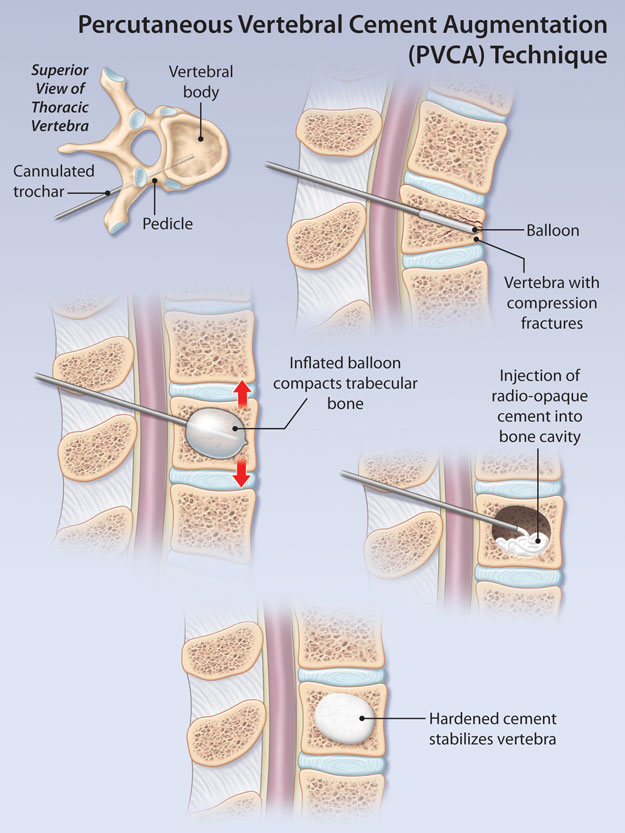
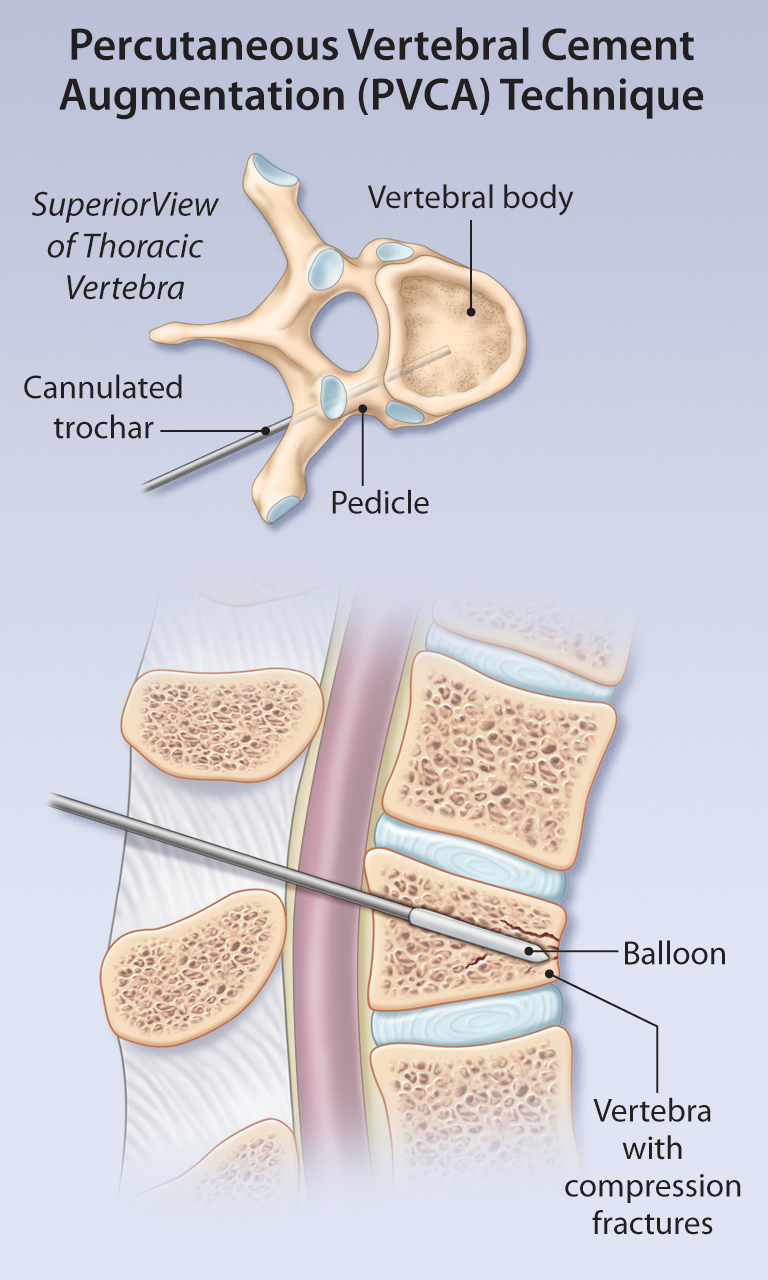
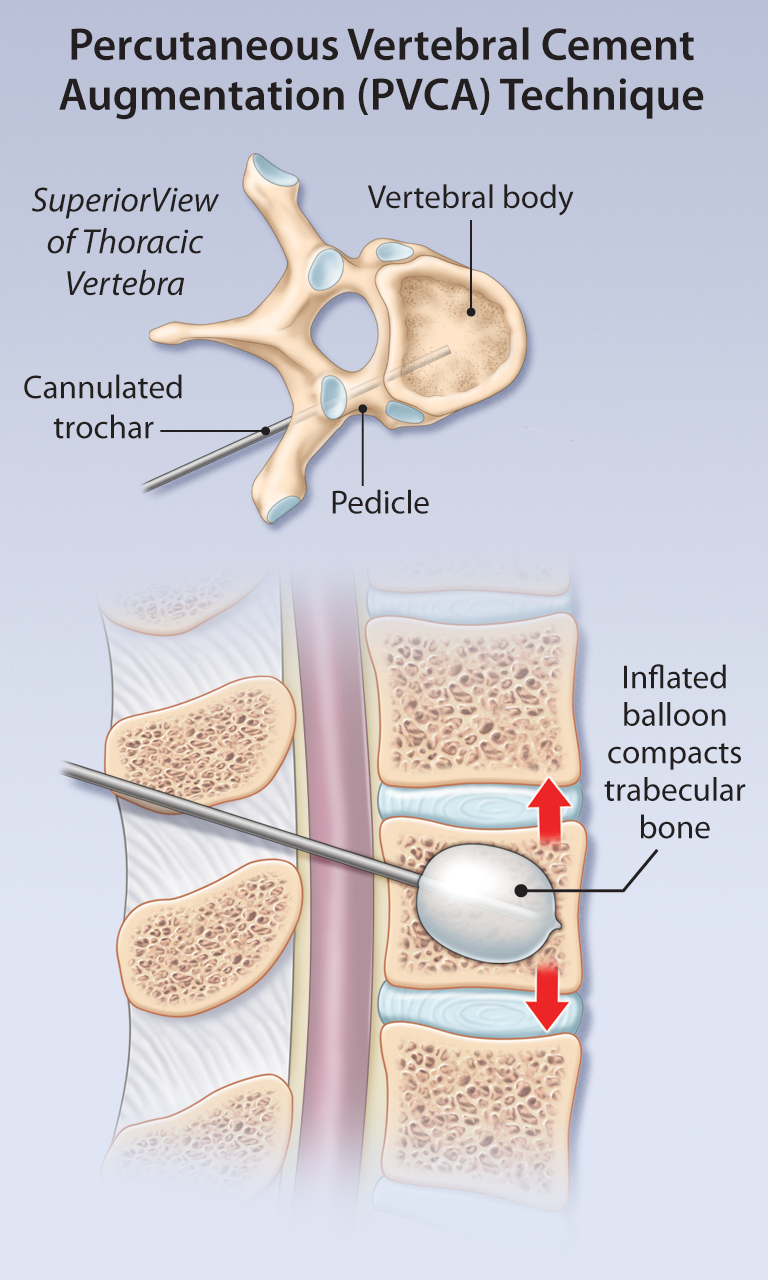
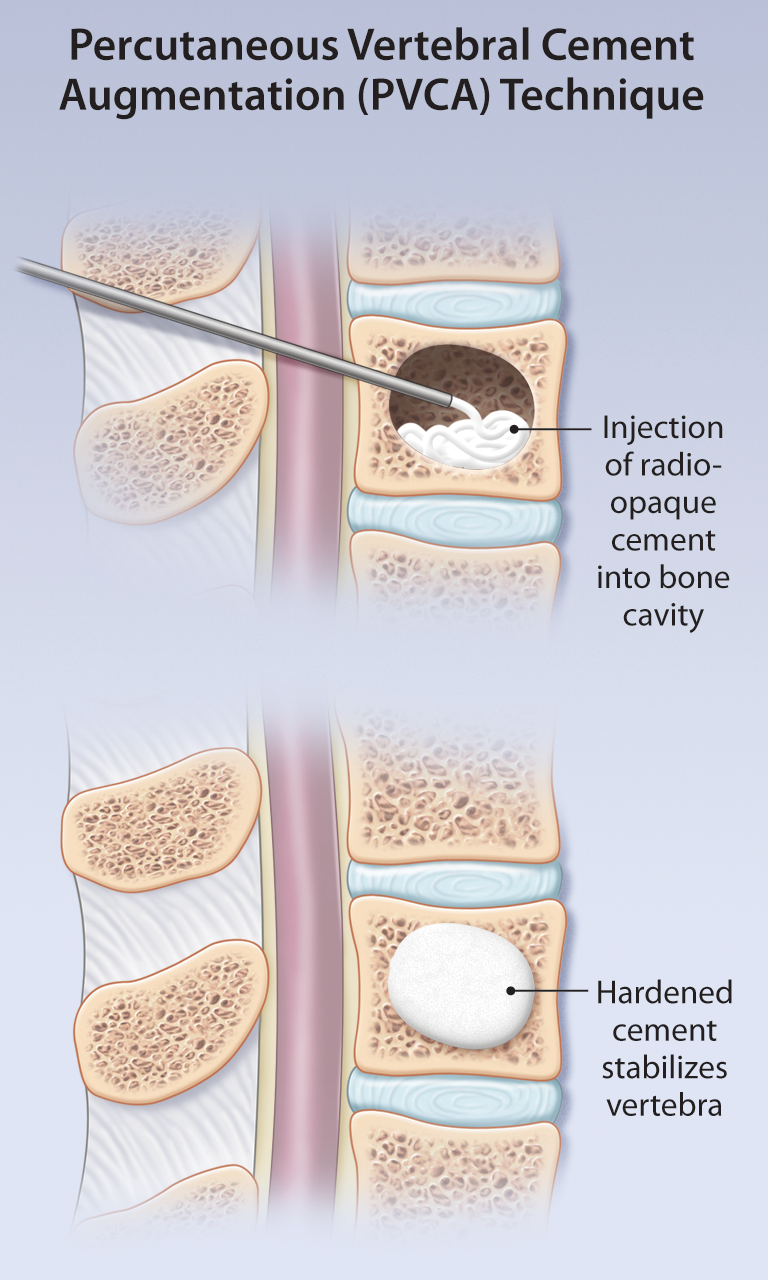
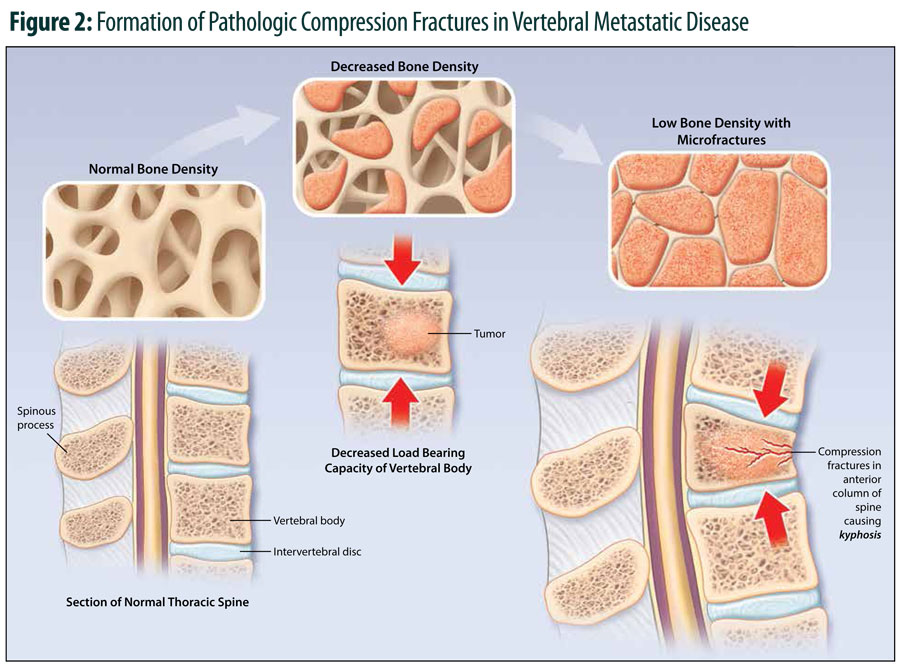
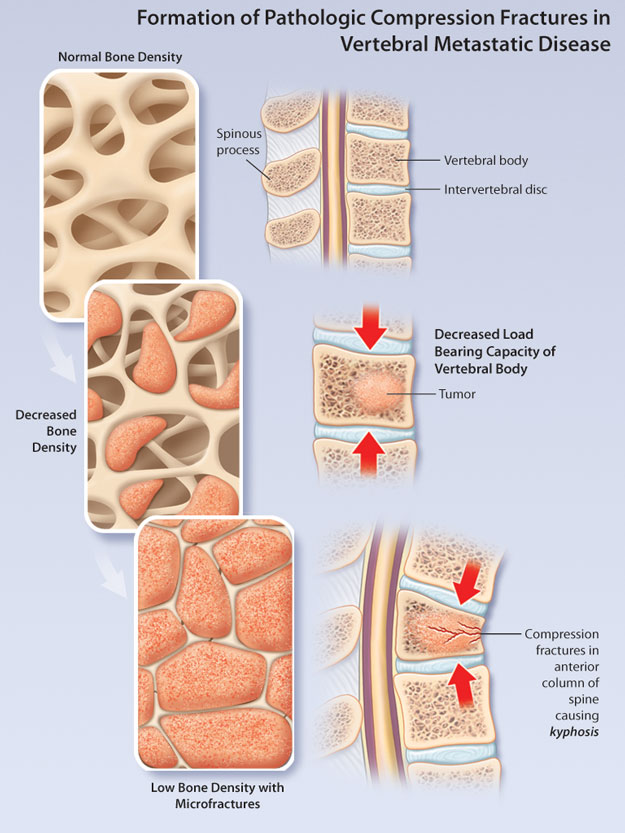
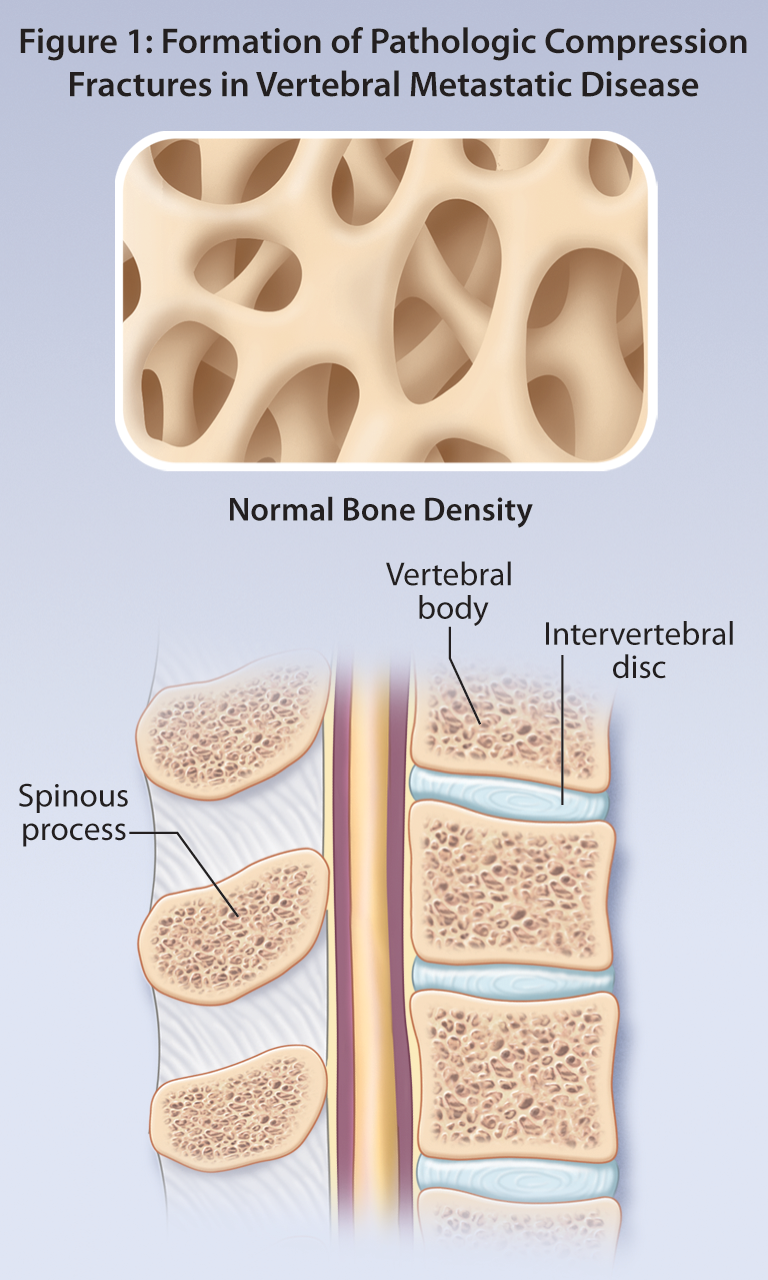
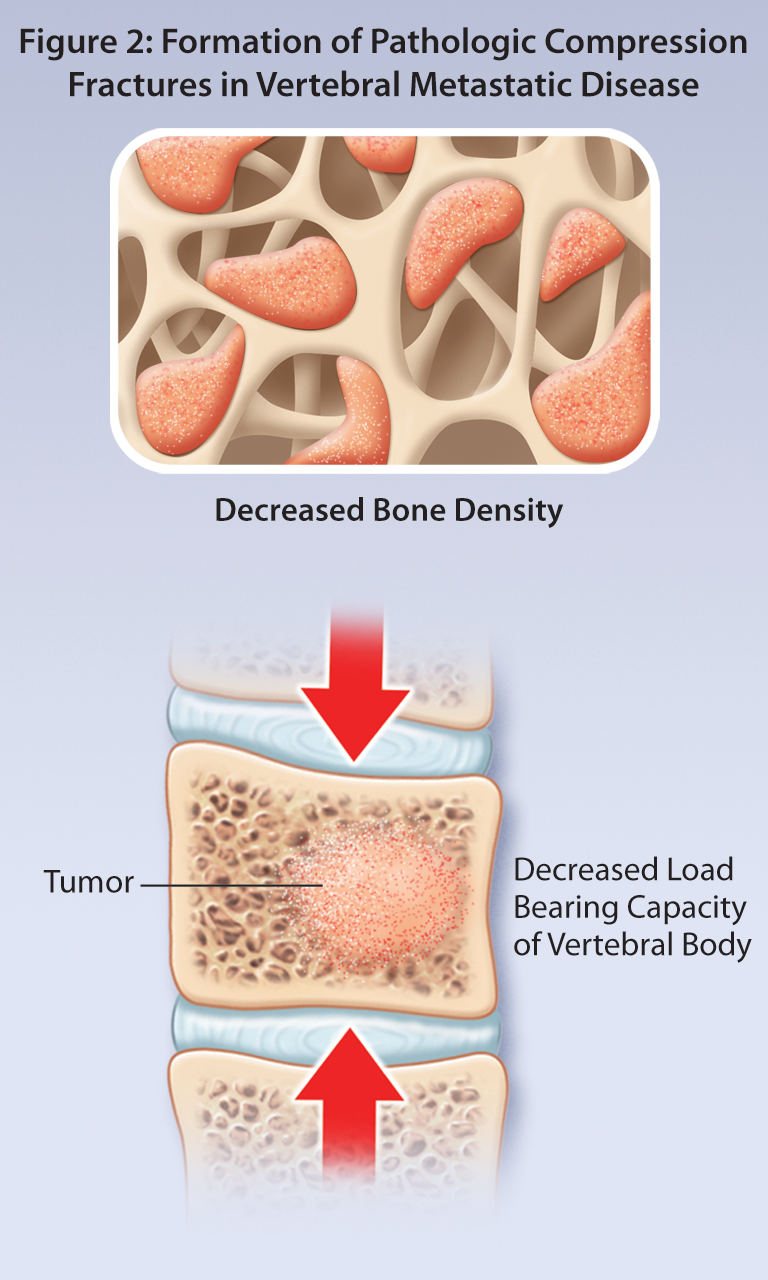
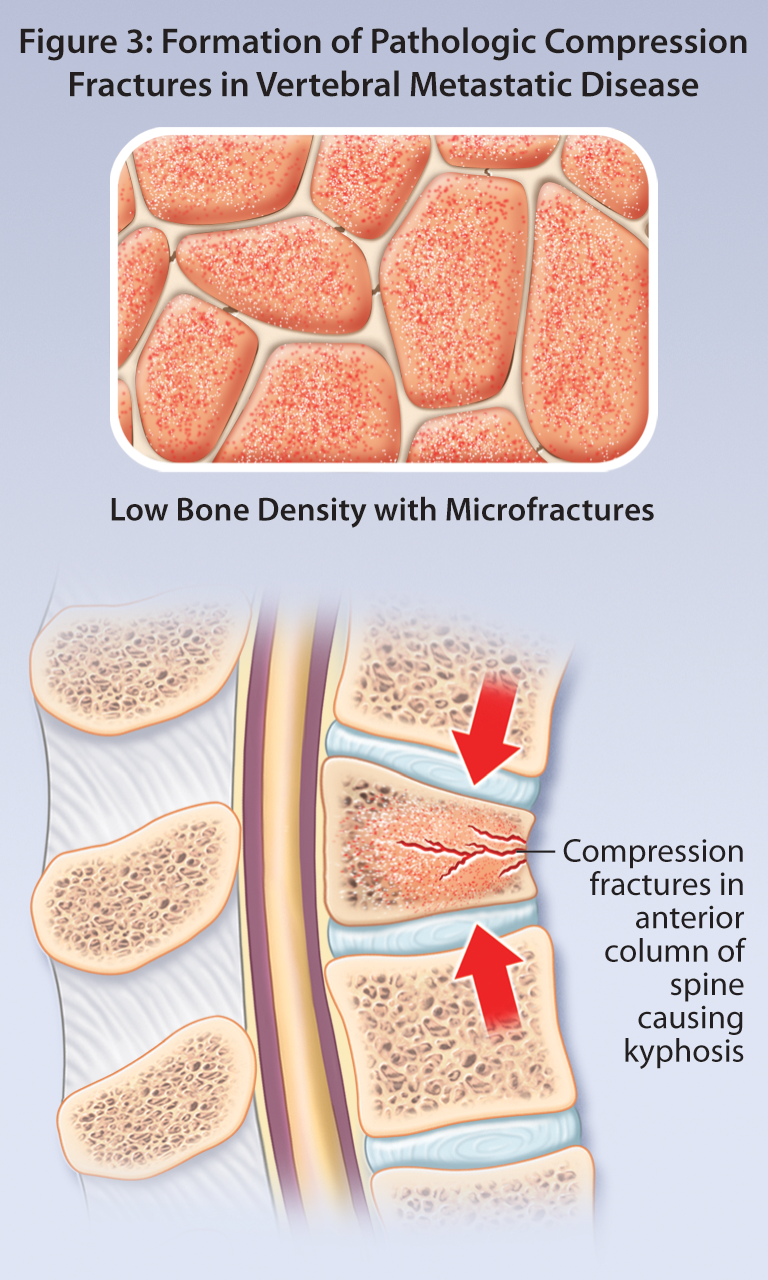
Vertebral Metastatic Disease: A Practice Guideline for the General Practitioner
Vertebral Metastatic Disease: A Practice Guideline for the General Practitioner
Error in Radiology: Negligence or Human Nature
D'Arcy Little, MD CCFP FRCPC, Chief of Diagnostic Imaging, Orillia Soldiers' Memorial Hospital,
Adjunct Clinical Lecturer, Department of Medical Imaging, University of Toronto, Toronto, ON,
Forensic Radiologist, Forensic Sciences and Coroners' Complex, Toronto, ON,
2015 Resident in Scientific Communications, Banff Centre, Banff, AB.
- Read more about Error in Radiology: Negligence or Human Nature
- Log in or register to post comments