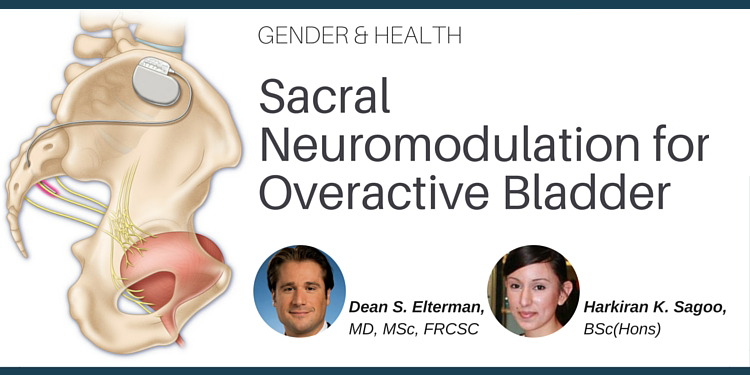
1Attending Urologic Surgeon, Toronto Western Hospital, University Health Network, Assistant Professor, Division of Urology, Department of Surgery, University of Toronto, Toronto, ON.
24th Year Medical Student at GKT School of Medicine, King's College London, U.K.