John W. DenBoer, MA, PhD1, Frederick L. Coolidge, PhD2, Daniel L. Segal, PhD3, & Sean Ahlmeyer, MA4,
1,2,3Department of Psychology, The University of Colorado at Colorado Springs (Colorado Springs, CO, USA).
4Colorado State Department of Corrections (Colorado Springs, CO, USA).
Abstract
The present study examined the personality and neuropsychological correlates of convicted male and female sex offenders. The investigators measured DSM-IV-TR psychopathology and neuropsychological dysfunction among rapists and child molesters using the Coolidge Axis II Inventory, a valid and reliable assessment instrument. Male child molesters displayed significantly higher Apathy scores than age-matched male controls. Male non-sexual offenders scored significantly higher than male child molesters, rapists, and controls on Histrionic Personality Disorder, Impulsivity, and Disinhibition. Female child molesters reported significantly elevated levels of psycho and neuropathology when compared to female non-offenders. Specifically, female child molesters reported greater Language Problems and Executive Dysfunction, along with greater levels of Psychoticism and Paranoia, when compared to female controls. The implications of these findings are discussed.
Key Words: personality, neuropsychology, sexual offenders, executive dysfunction, child molestation, rape.

 Michael Gordon, MD, MSc, FRCPC, Medical Program Director, Palliative Care, Baycrest Geriatric Health Care System, Professor of Medicine, University of Toronto, Toronto, ON.
Michael Gordon, MD, MSc, FRCPC, Medical Program Director, Palliative Care, Baycrest Geriatric Health Care System, Professor of Medicine, University of Toronto, Toronto, ON.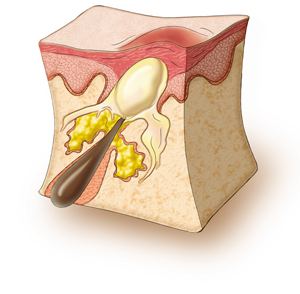 Human skin is covered in hundreds of thousands of microscopic hair follicles, called pores. These are particularly prominent on the face, neck, back, and chest. These pores are connected to oil glands under the skin that make a substance called sebum. Sometimes these follicles produce too many cells and become blocked. As a result, sebum (oil) gets trapped and bacteria (P. acnes) begin to grow.1,2,4
Human skin is covered in hundreds of thousands of microscopic hair follicles, called pores. These are particularly prominent on the face, neck, back, and chest. These pores are connected to oil glands under the skin that make a substance called sebum. Sometimes these follicles produce too many cells and become blocked. As a result, sebum (oil) gets trapped and bacteria (P. acnes) begin to grow.1,2,4 Treatment for acne has several goals: to heal pimples, to prevent pimples (by decreasing sebum production, killing bacteria, and normalizing skin shedding), and to prevent scarring.1,6
Treatment for acne has several goals: to heal pimples, to prevent pimples (by decreasing sebum production, killing bacteria, and normalizing skin shedding), and to prevent scarring.1,6