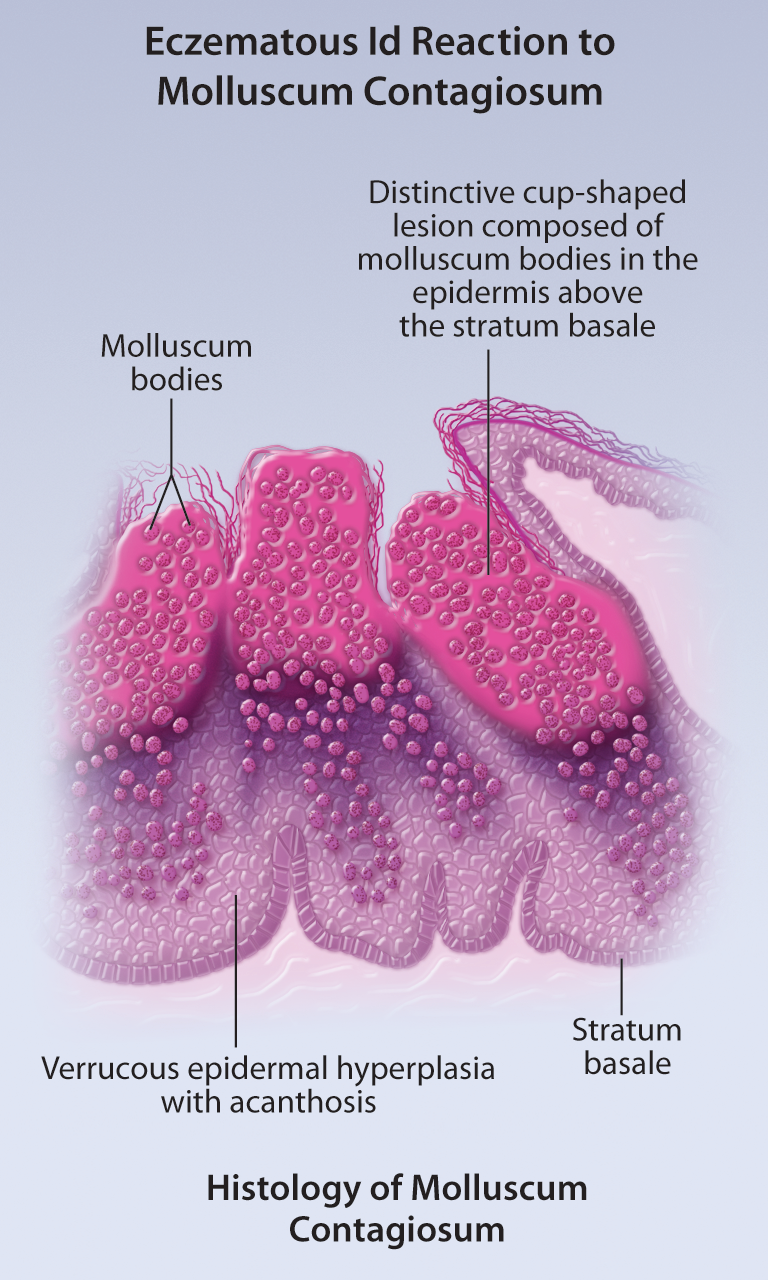
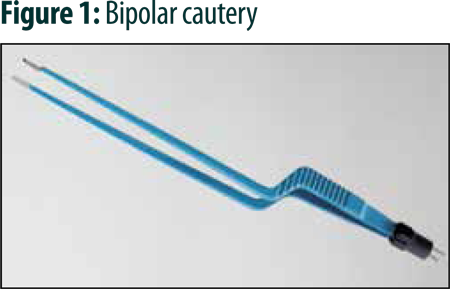
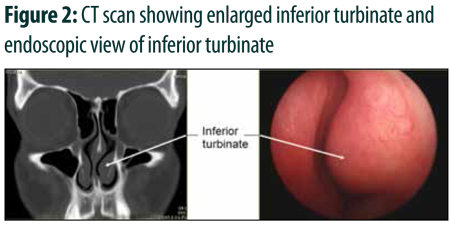
Bipolar Electrofulgration with Endoscopic Approach in Allergic Turbinates
Bipolar Electrofulgration with Endoscopic Approach in Allergic Turbinates
Editor's Note, Volume 5 Issue 4
Editor's Note, Volume 5 Issue 4
D’Arcy Little, MD, CCFP, FRCPC
Medical Director, JCCC and HealthPlexus.NET

- Read more about Editor's Note, Volume 5 Issue 4
- Log in or register to post comments
Post-test: Vertebral Metastatic Disease: A Practice Guideline for the General Practitioner
Members of the College of Family Physicians of Canada may claim MAINPRO-M2 Credits for this unaccredited educational program.
| Questions | 5 |
|---|---|
| Attempts allowed | Unlimited |
| Available | Always |
| Backwards navigation | Forbidden |
You are not allowed to take this Quiz.
Pre-test: Vertebral Metastatic Disease: A Practice Guideline for the General Practitioner
| Questions | 4 |
|---|---|
| Attempts allowed | Unlimited |
| Available | Always |
| Pass rate | 75 % |
| Backwards navigation | Allowed |
You are not allowed to take this Quiz.
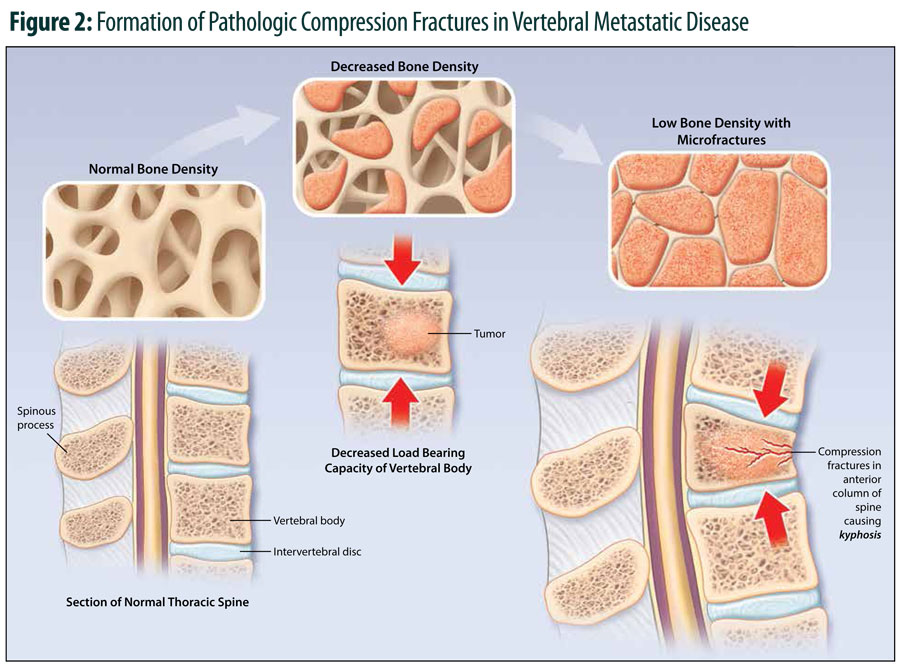
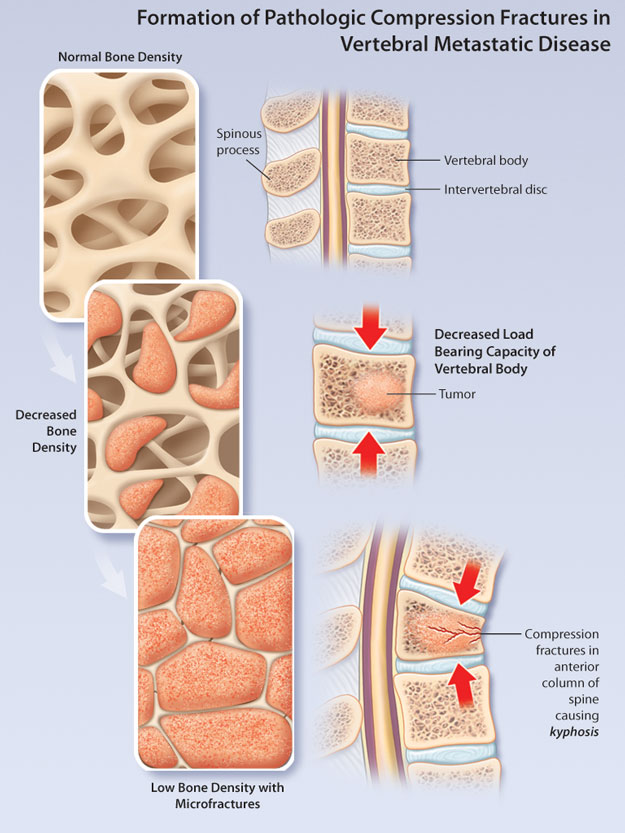
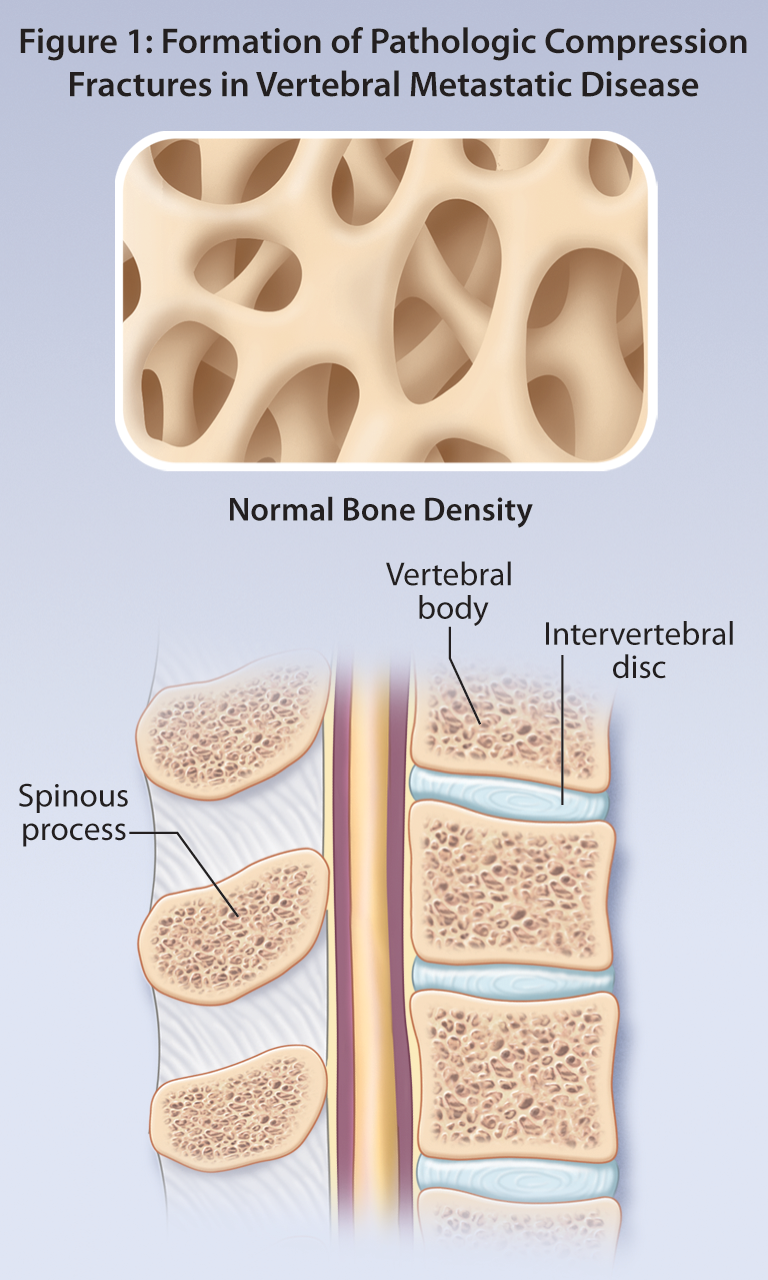
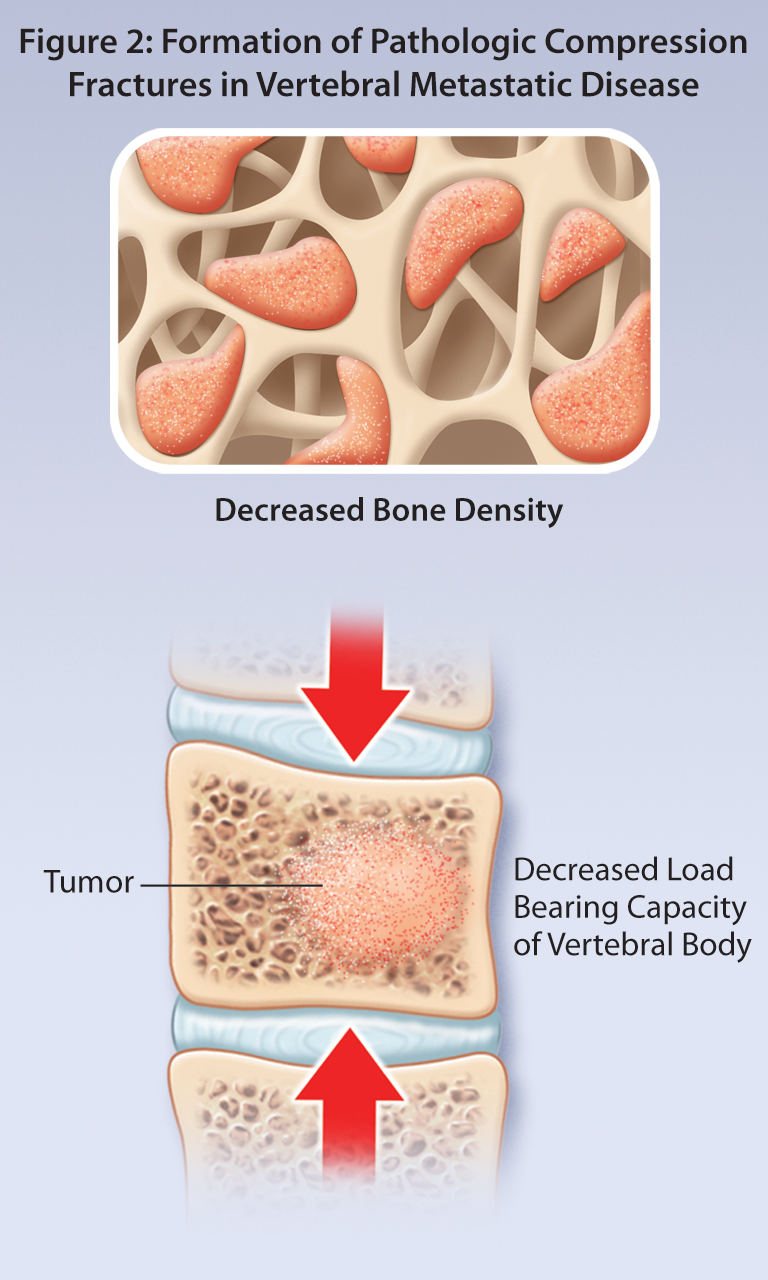
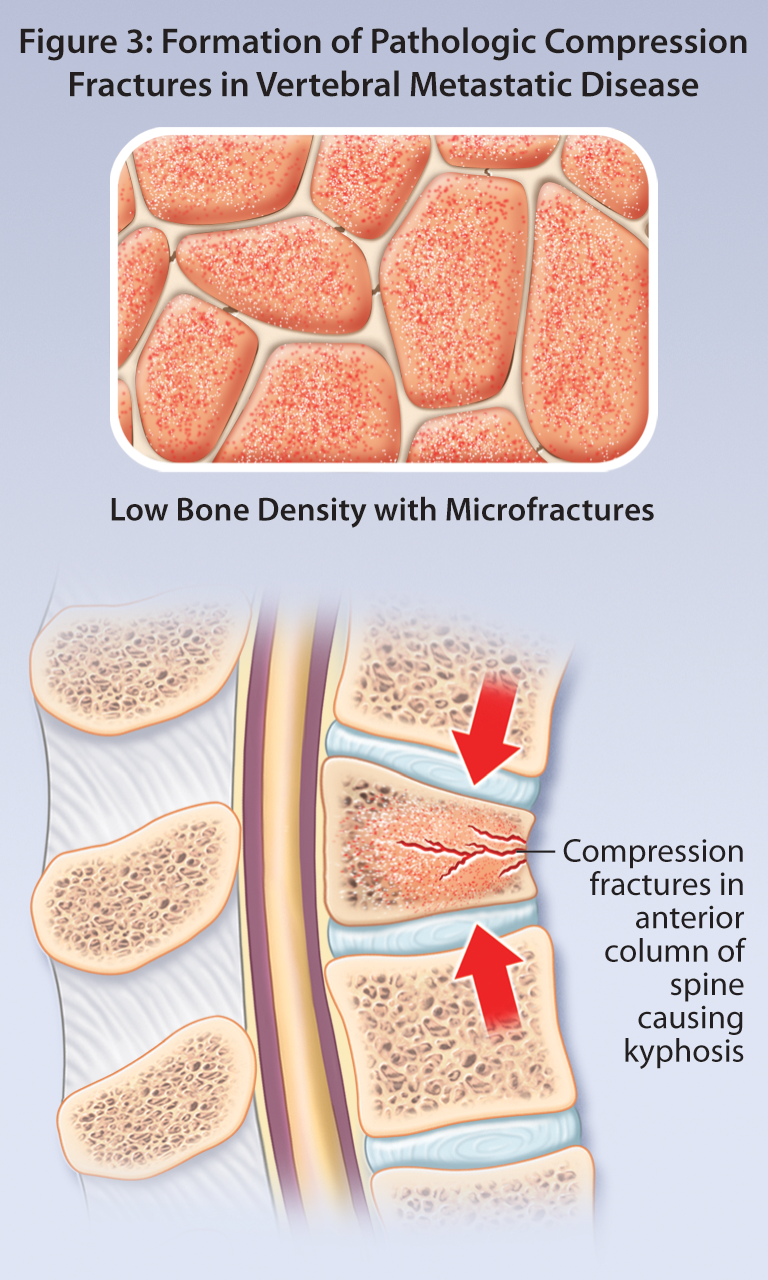
Vertebral Metastatic Disease: A Practice Guideline for the General Practitioner
Vertebral Metastatic Disease: A Practice Guideline for the General Practitioner
Error in Radiology: Negligence or Human Nature
D'Arcy Little, MD CCFP FRCPC, Chief of Diagnostic Imaging, Orillia Soldiers' Memorial Hospital,
Adjunct Clinical Lecturer, Department of Medical Imaging, University of Toronto, Toronto, ON,
Forensic Radiologist, Forensic Sciences and Coroners' Complex, Toronto, ON,
2015 Resident in Scientific Communications, Banff Centre, Banff, AB.
- Read more about Error in Radiology: Negligence or Human Nature
- Log in or register to post comments
Tales of Heartache and Woe
Editor's Note, Volume 5 Issue 3
Editor's Note, Volume 5 Issue 3
D’Arcy Little, MD, CCFP, FRCPC
Medical Director, JCCC and HealthPlexus.NET

- Read more about Editor's Note, Volume 5 Issue 3
- Log in or register to post comments