Diagnostic Radiology in Low Back Pain
Diagnostic Radiology in Low Back Pain
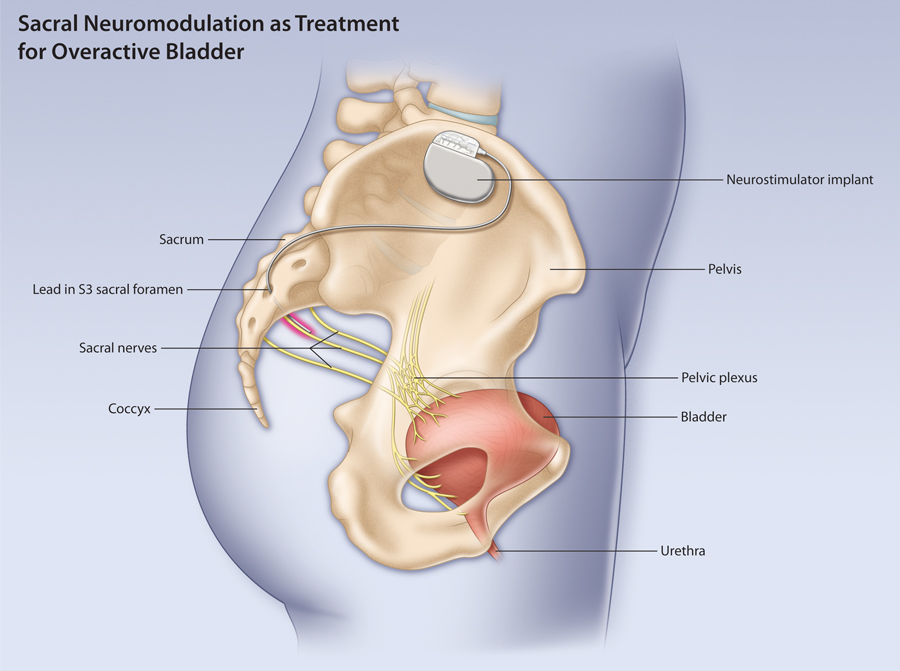
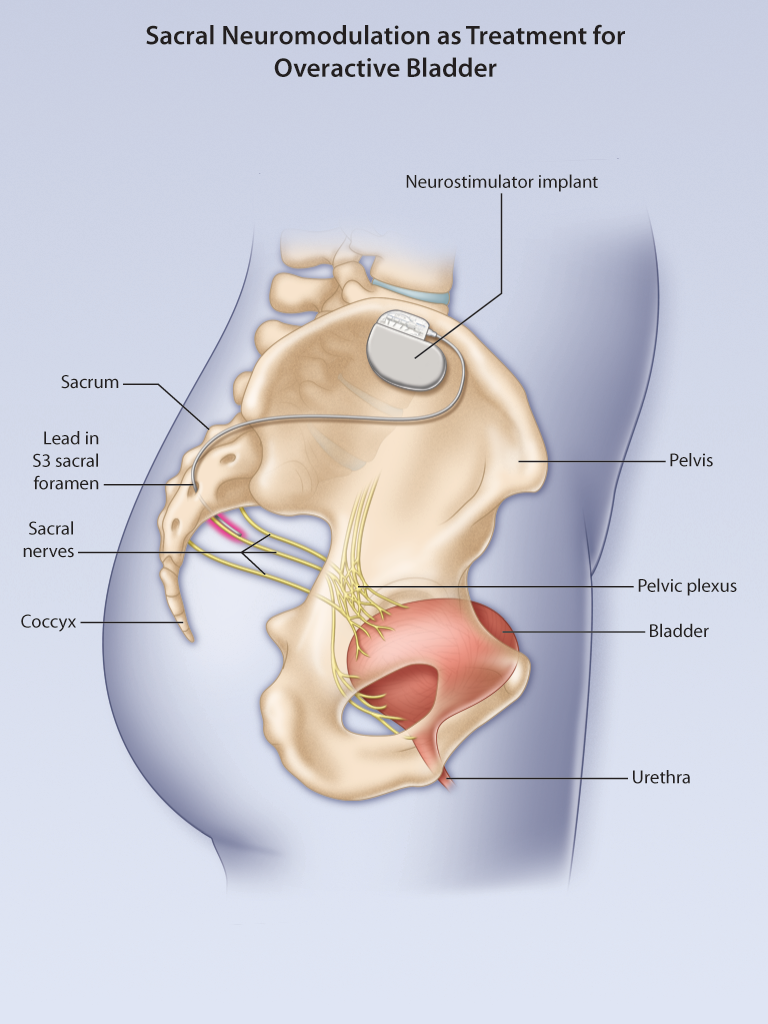
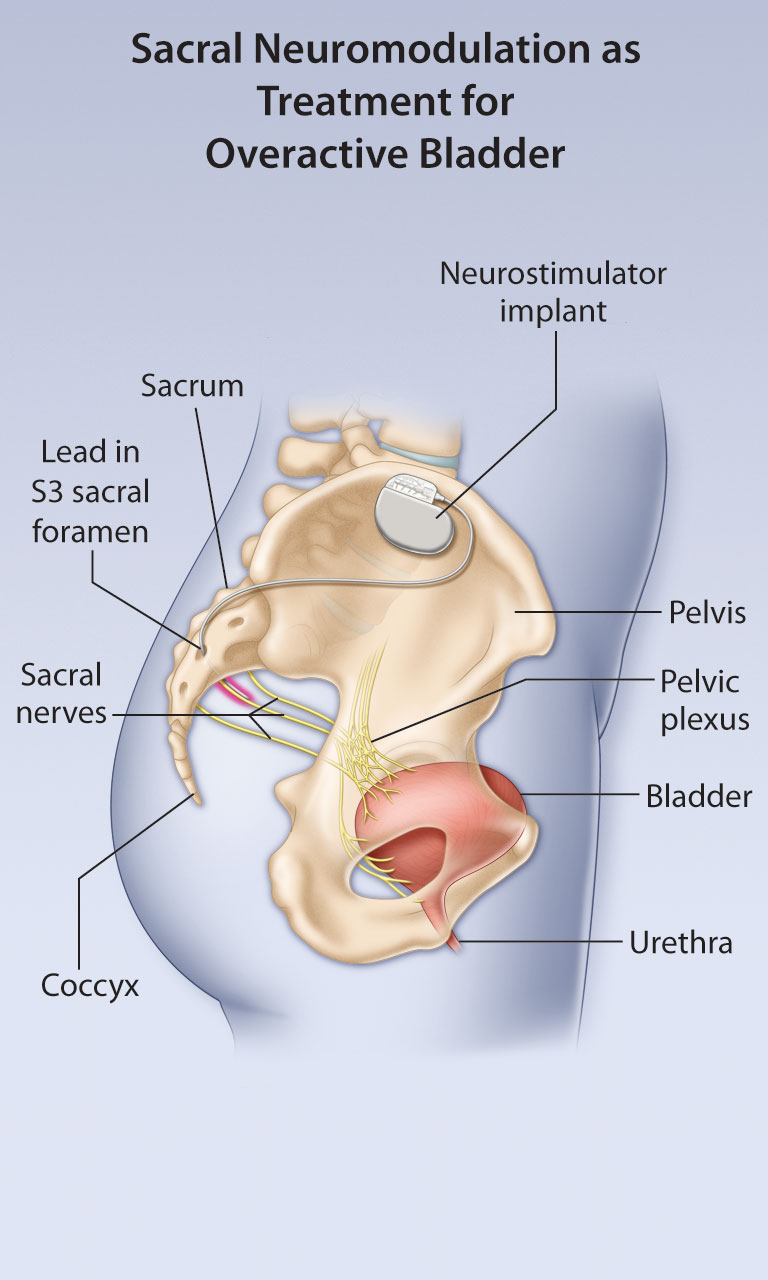
Sacral Neuromodulation for Overactive Bladder
Post-test: Sacral Neuromodulation for Overactive Bladder
Members of the College of Family Physicians of Canada may claim MAINPRO-M2 Credits for this unaccredited educational program.
| Questions | 5 |
|---|---|
| Attempts allowed | Unlimited |
| Available | Always |
| Backwards navigation | Forbidden |
You are not allowed to take this Quiz.
Pre-test: Sacral Neuromodulation for Overactive Bladder
| Questions | 3 |
|---|---|
| Attempts allowed | Unlimited |
| Available | Always |
| Pass rate | 75 % |
| Backwards navigation | Allowed |
You are not allowed to take this Quiz.
Post-test: Diagnostic Radiology in Low Back Pain
Members of the College of Family Physicians of Canada may claim MAINPRO-M2 Credits for this unaccredited educational program.
| Questions | 5 |
|---|---|
| Attempts allowed | Unlimited |
| Available | Always |
| Backwards navigation | Forbidden |
You are not allowed to take this Quiz.
Pre-test: Diagnostic Radiology in Low Back Pain
| Questions | 3 |
|---|---|
| Attempts allowed | Unlimited |
| Available | Always |
| Pass rate | 75 % |
| Backwards navigation | Allowed |
You are not allowed to take this Quiz.
Editor's Note, Volume 5 Issue 2
Editor's Note, Volume 5 Issue 2
D’Arcy Little, MD, CCFP, FRCPC
Medical Director, JCCC and HealthPlexus.NET

- Read more about Editor's Note, Volume 5 Issue 2
- Log in or register to post comments