Pediatric Psoriasis
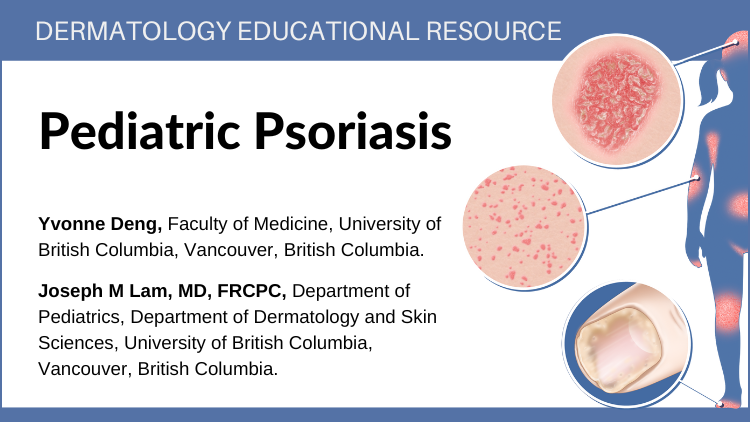
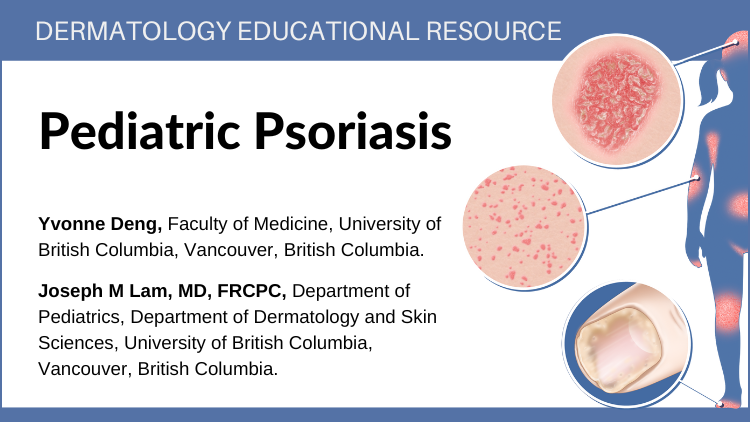
Psoriasis is a common but chronic skin condition that causes
inflammation and scaling (red elevated patches and flaking silvery
scales). The patches can be itchy or sore, causing discomfort and pain.
Psoriasis causes skin cells to rise to the surface and shed at a very
rapid rate. On average, people with psoriasis shed their skin cells
every 3 to 4 days, while people without the condition have a turnover
rate of about every 30 days.1,2,3,4