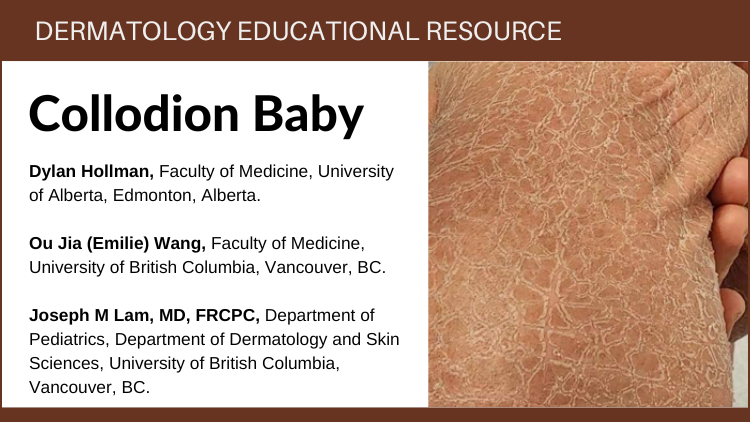
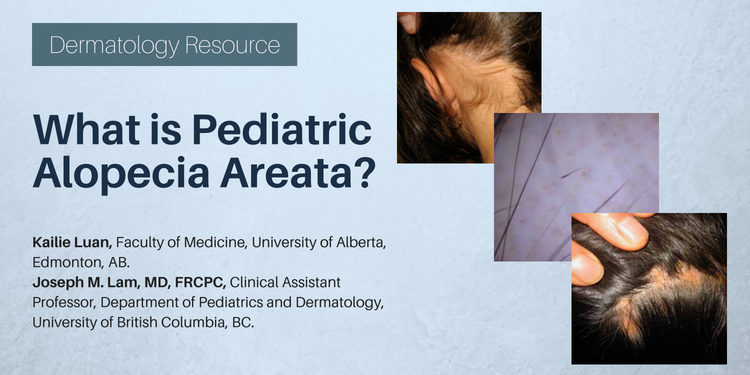
1Faculty of Medicine, University of Alberta.2 Faculty of Medicine, University of British Columbia, Vancouver, British Columbia, Canada.
3Department of Pediatrics, Department of Dermatology and Skin Sciences, University of British Columbia, Vancouver, British Columbia, Canada.