Angela M. Cheung, MD, PhD, FRCP(C), CCD, Director, Osteoporosis Program, University Health Network and Mount Sinai Hospital; Associate Director, Women’s Health Program, University Health Network; Associate Professor, University of Toronto, Toronto,ON.
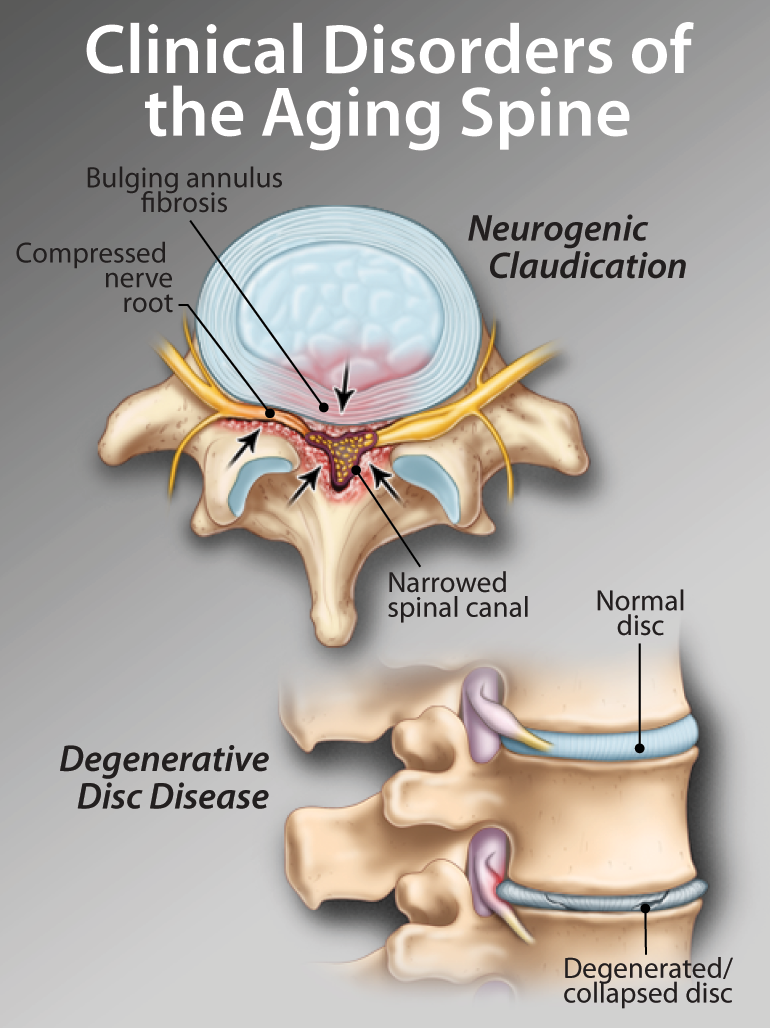
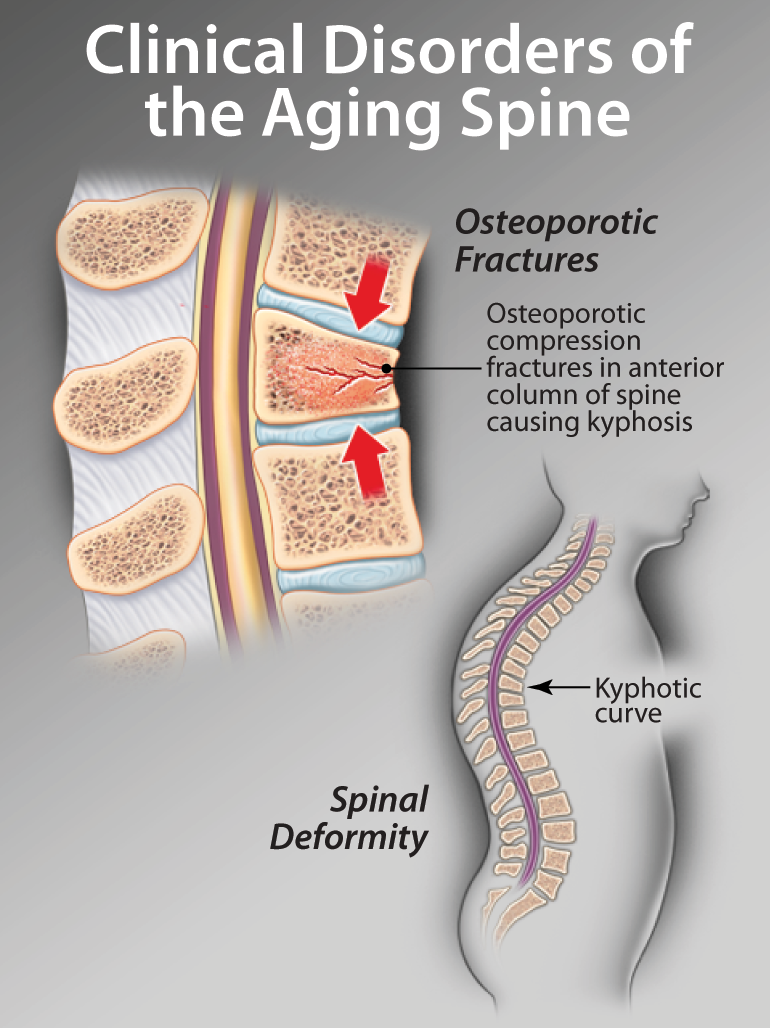
Osteoporosis is common in postmenopausal women and older men. There are various efficacious therapies for the treatment of osteoporosis and the prevention of osteoporotic fractures in Canada. First-line therapies include alendronate, risedronate and raloxifene; all of these are oral antiresorptive therapies. In this article, we review new drug therapies currently or soon to be available in Canada, such as bone formation therapies (parathyroid hormone and strontium ranelate) and intravenous infusions (such as zoledronic acid), and compare them to existing therapies.
Key words: osteoporosis, osteoporotic fractures, parathyroid hormone, strontium, zoledronic acid.