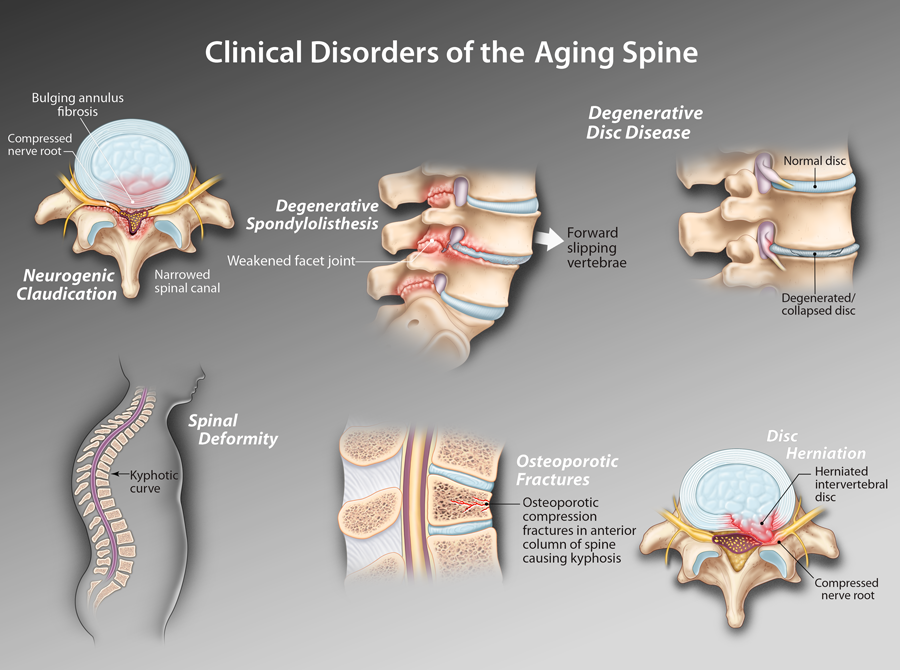
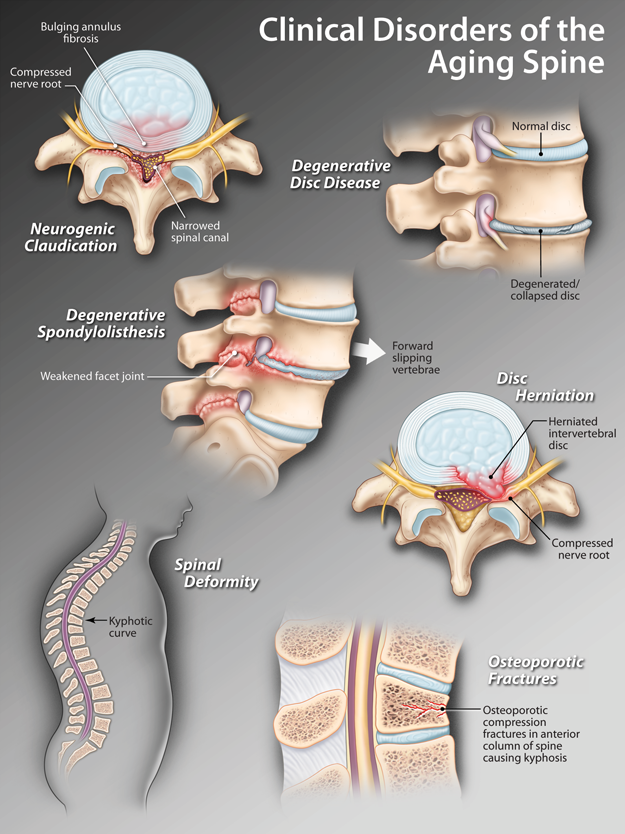
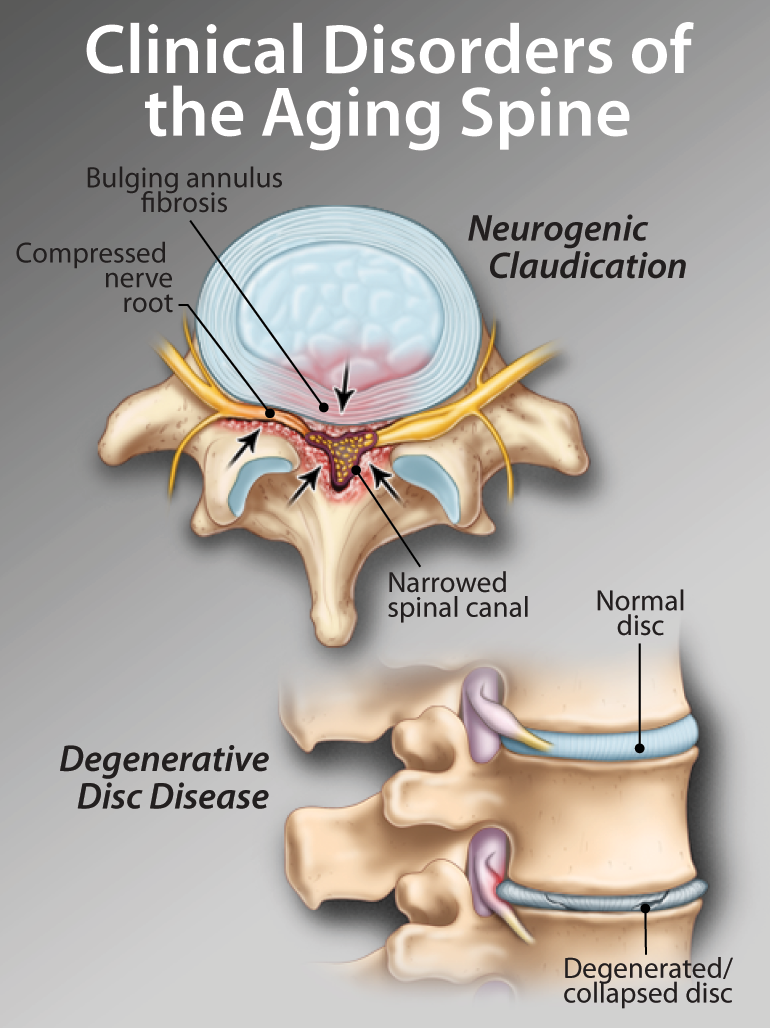
| The diagnosis of neurogenic claudication is made on the history of intermittent leg dominant pain brought on by activity, usually walking, and relieved by rest in flexion, usually by sitting down. The physical examination while the patient is at rest is often normal. |
| Mechanical back pain associated with disc degeneration is seldom an indication for surgery and can usually be adequately managed through a combination of education, activity modification, general fitness and exercises selectively tailored to improve the pain-producing positons and movements. |
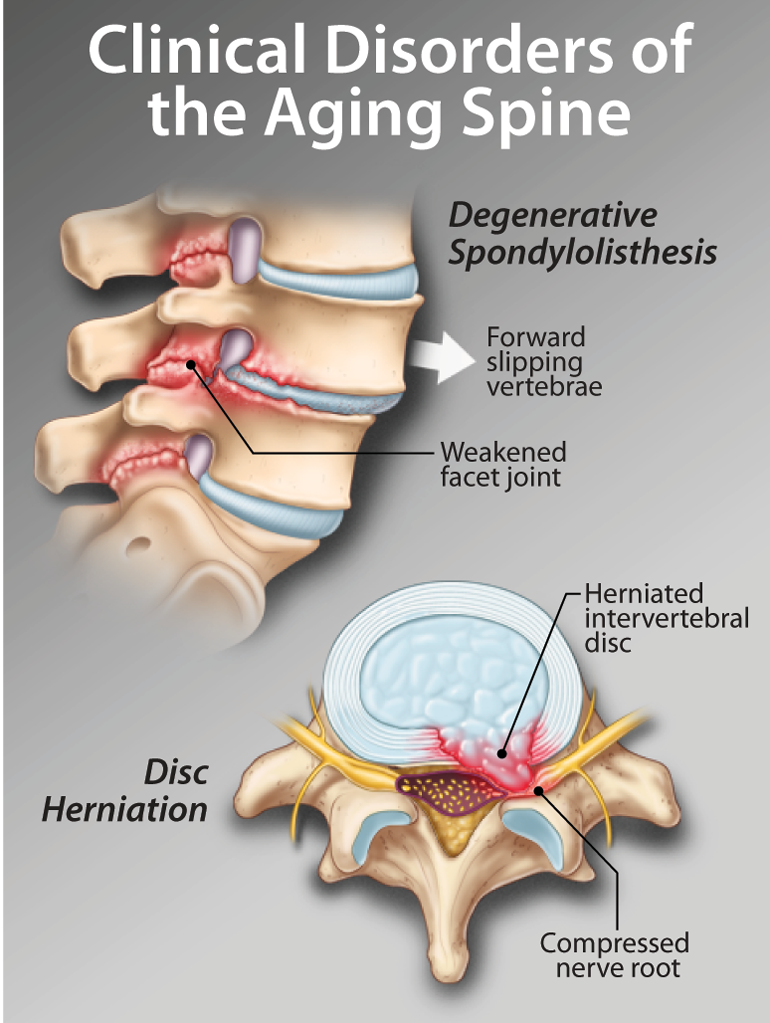
| Disc herniation producing acute sciatica is uncommon in the older patient and the diagnosis should be made with caution. True radicular pain is constant and leg dominant. Referred, intermittent leg pain frequently accompanies back dominant pain and should not be treated as sciatica. |
| Enduring spine surgery is a major challenge for the elderly patient. The decision to operate must be made after comprehensive consultation, emphasizing the prolonged recovery and weighing the potential benefits against the inevitable risks, including the risk to life. |