Improving the Lives of Your Aging Male Patients: Considering Whether Testosterone Plays a Meaningful Role
Testosterone and the Prostate
Speaker: Gerald Brock, MD, FRCSC, Professor, Department of Surgery, Division of Urology, University of Western Ontario, London, ON.
In men receiving androgen replacement therapy, the safety aspects regarding the prostate are an area of clinical importance. Dr. Gerald Brock expressed the hope that his discussion “Testosterone and the Prostate” would contribute to greater understanding, counter prevalent misinformation, and support the growing consensus that having low testosterone has adverse health consequences. Low testosterone does not confer protective effects against prostate cancer, and treatment of hypogonadal men does not elevate prostate cancer risk, he stated.
What are the risks and benefits of treating hypogonadal patients? Dr. Brock offered an illustrative case study and queried the audience about their attitudes toward treatment with exogenous testosterone.
Dr. Brock questioned whether his example patient—a 56-year-old experiencing loss of sexual drive, low energy, and mild erectile dysfunction—would be considered by his listeners to be a good candidate for supplemental testosterone. The patient has been seen previously for hypertension and elevated cholesterol, is on hypertension medication, and has mild benign prostatic hypertrophy symptoms. Further, he has a family history of prostate cancer and his last prostate-specific antigen (PSA) was 2.2ng/dl; his digital rectal exam (DRE) is normal. On testing, his total testosterone returns at 5 (N=6–26).
The audience’s response suggested widespread reluctance to treat with supplemental testosterone in this patient’s case, despite having the appropriate symptom profile. Further, he reminded audience members, testosterone improves many of the physical endpoints of concern that Dr. Jeremy Gilbert and Dr. Juan Carlos Monge spoke of.
Dr. Brock inferred from the hesitancy that the presumed risk-benefit profile of supplemental testosterone constrains clinical practice. He hoped the information he provided would support their clinical judgement as to who to treat and who to exclude from treatment.
He reviewed data from the Baltimore Longitudinal Study of Aging that hypogonadism increases with age, and that the percentage of men with hypogonadism increases progressively after age 50 years.1
Studies show that low total testosterone levels predicts development of worsening risk factors for the metabolic syndrome and diabetes. These findings indicate that hypoandrogenism is an early marker for perturbations in insulin and glucose metabolism that may progress to metabolic syndrome or frank diabetes.2 Further, a study from Shores et al. found that survival times were shorter in men with low or equivocal testosterone levels than in those with normal testosterone levels.3 All-cause mortality was 34.9% in men with low testosterone levels, 24.6% in men with equivocal testosterone levels, and 20.1% in men with normal testosterone levels.
Despite the positive evidence presented as to the inverse and favourable relationship between plasma testosterone and cardiovascular events as well as metabolic risk factors, he understood that compromising cancer risk was a strong and mitigating concern for those in clinical practice. Dr. Brock assured that supplemental testosterone posed no impact on those hypogonadal men with nonconcerning exam and lab profiles. From an overall health perspective, study evidence suggests hypogonadal patients will likely experience concrete benefits.
The common view that higher testosterone represents a risk factor for prostate cancer has little evidentiary support, Dr. Brock stated. Data show that cancer occurs at least as commonly in men with low testosterone as in men with higher levels. Indeed, recent evidence suggests that those men with low testosterone are likely to have aggressive prostate cancer. A recent study’s investigators concluded that the risk of prostate cancer was doubled for men with the lowest testosterone values.4 Further, the form of testosterone given does not change the risk level: studies of hypogonadal men receiving testosterone therapy using transdermal, topical, intramuscular injection, or a combination of these preparations have demonstrated a low frequency of prostate cancer.5
Dr. Brock reviewed study data showing that if a patient is on a longer-term testosterone regimen, his PSA level may indeed increase slightly (although many studies do not show this), but only to the level of a eugonadal man.6 Test results will show a modest increase in hemoglobin, in hematocrit, but on the positive side, his scores on the Aging Male Symptom Scale improve. Ultimately, investigations of testosterone’s impact on prostate tissue have shown no change in prostatic androgen concentration. In most cases, any increase in PSA seen will stay in normal range.
He reminded the audience that the Endocrine Society’s clinical practice guideline recommends a DRE of the prostate and measurement of PSA before initiating testosterone therapy. In assessing prostate health, family history is very important. Having a first-degree relative with prostate cancer doubles a patient’s risk. From his perspective and the weight of the evidence, it is not a concern to treat hypogonadal men with testosterone as long as they are closely followed. Some data suggest that actual risk lies in that segment of patients with lower testosterone levels, who may be at risk for higher grade prostate cancer.7
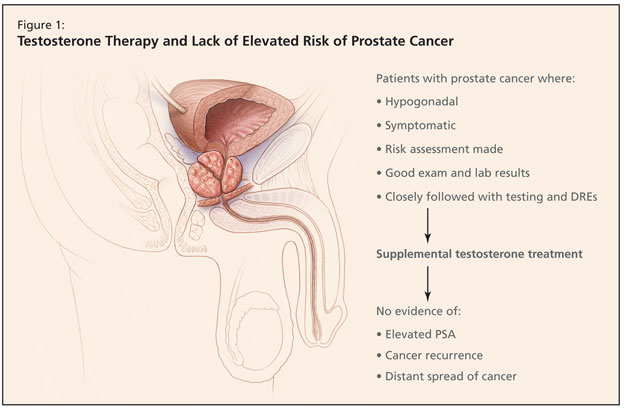
Dr. Brock emphasized that he should not be understood as advocating that physicians treat their patients with prostate cancer with testosterone, but if they choose to do so, in cases where men are hypogonodal and symptomatic and a risk assessment is made, there are still no grounds for concern that supplemental testosterone is perilous. Provided the patient is symptomatic, has good exam and lab results, and is closely followed with testing and DREs, treatment is not unsafe. Studies have shown that hypogonadal men treated with androgen replacement therapy show no evidence of elevated PSA, cancer recurrence, or distant spread of cancer (Figure 1).8,9
In closing, Dr. Brock emphasized that eugonadal testosterone levels are important for good overall health and sexual well-being. Clinical benefits of testosterone therapy include improved libido, erectile function, better cardiovascular health, reduced metabolic syndrome risk factors, and better body composition. There is no evidence that testosterone increases prostate cancer risk, and some evidence suggests that hypogonadism increases aggressive prostate cancer risk. It is increasingly understood that hypogonadism and not its treatment is correlated with multiple poor health outcomes, and is a diagnosis of true concern.
References:
-
Harman SM, Metter EJ, Tobin JD, Pearson J, Blackman MR; Baltimore Longitudinal Study of Aging. Longitudinal effects of aging on serum total and free testosterone levels in healthy men. J Clin Endocrinol Metab 2001;86:724–31.
-
Laaksonen DE, Niskanen L, Punnonen K, et al. Testosterone and sex hormone-binding globulin predict the metabolic syndrome and diabetes in middle-aged men. Diabetes Care 2004;27:1036–41.
-
Shores MM, Matsumoto AM, Sloan KL, et al.. Low serum testosterone and mortality in male veterans. Arch Intern Med 2006;166:1660–5.
-
Morgentaler A, Rhoden EL. Prevalence of prostate cancer among hypogonadal men with prostate-specific antigen levels of 4.0 ng/mL or less. Urology 2006;68:1263–7.
-
Rhoden EL, Morgentaler A. Risks of testosterone-replacement therapy and recommendations for monitoring. N Engl J Med 2004;350:482–92.
-
Saad F, Gooren LJ, Haider A, Yassin A. A dose-response study of testosterone on sexual dysfunction and features of the metabolic syndrome using testosterone gel and parenteral testosterone undecanoate. J Androl 2008;29:102–5.
-
Schatzl G, Madersbacher S, Thurridl T, et al. High-grade prostate cancer is associated with low serum testosterone levels. Prostate 2001;47:52–8.
-
Agarwal PK, Oefelein MG. Testosterone replacement therapy after primary treatment for prostate cancer. J Urol 2005;173:533–6.
-
Kaufman JM, Graydon RJ. Androgen replacement after curative radical prostatectomy for prostate cancer in hypogonadal men. J Urol 2004;172:920–22.
Sponsored by an unrestricted educational grant from Solvay Pharma Inc.