Improving the Lives of Your Aging Male Patients: Considering Whether Testosterone Plays a Meaningful Role
Discussing the Association between Cardiovascular Risk and Hypogonadism
Speaker: Juan Carlos Monge, MD, FRCPC, FACC, Associate Professor of Medicine, University of Toronto; Division of Cardiology, St. Michael’s Hospital, Toronto, ON.
Dr. Juan Carlos Monge spoke about the role of testosterone in the regulation of the cardiovascular system, as well as about the effects of hypogonadism and testosterone replacement on some cardiovascular risk factors. He discussed the experimental and clinical evidence concerning testosterone deficiency and testosterone replacement therapy’s effects on the cardiovascular system and metabolic risks, effects on lipoprotein metabolism, direct arterial effects, and effects on body composition, as well as relevant data from the oncology literature on the consequences of androgen deprivation therapy.
Generally, most data show an inverse, favourable relationship between plasma testosterone and cardiovascular events. Testosterone functions in the cardiovascular system via androgen receptors. Some of the activities of testosterone in the cardiovascular system depend on the endothelium. Testosterone activates nitric oxide synthase (NOS); NOS, which was first characterized as a vasodilator, is the hallmark of endothelial health. Bioavailable NOS promotes good health as it has fibrinolytic activity and is antithrombotic and antiproliferative. The cardiovascular risk factors in general decrease the bioavailability of NOS. Smoking, hypertension, and dyslipidemia all have deleterious effects on NOS. Testosterone parallels the dilatory effects of NOS.
Some of testosterone’s effects are mediated by estrogen as aromatizable forms of testosterone are converted to estradiol, which has cardioprotective antioxidant effects. There are also effects on the level of lipoprotein production and a correlation with lowered LDL cholesterol, decreased central obesity, etc.
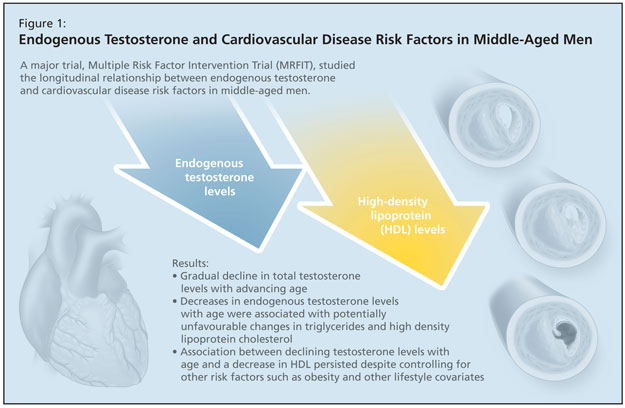
Dr. Monge discussed a study of the longitudinal relationship between endogenous testosterone and cardiovascular disease risk factors in middle-aged men, which followed the Multiple Risk Factor Intervention Trial (MRFIT) participants (Figure 1).1 This was a large trial of 400,000 US patients between 40–60 years of age who were followed for 13 years to determine if changes in total testosterone related to changes in cardiovascular disease risk factors. Published results reported a gradual decline in total testosterone levels with advancing age. Decreases in endogenous testosterone levels with age in men were associated with potentially unfavourable changes in triglycerides and high density lipoprotein cholesterol, according to the authors. The association between declining testosterone levels with age and a decrease in HDL persisted despite controlling for other risk factors such as obesity and other lifestyle covariates.
Dr. Monge also reviewed a study by Feldman et al., using data from the Massachusetts Male Aging Study, on the adrenal steroid dehydroepiandrosterone (DHEA) and its sulfate (DHEAS), which have been characterized as protective against ischemic heart disease (IHD) in men.2 The study investigated whether serum levels of DHEA or DHEAS could predict incident IHD over a 9-year interval. The authors reported an association between low testosterone levels and IHD: study participants with serum DHEAS in the lowest quartile at baseline (<1.6 microg/ml) were significantly more likely to incur IHD by follow-up (adjusted odds ratio = 1.60, 95 percent confidence interval: 1.07, 2.39; p = 0.02), independently of known risk factors including age, obesity, diabetes, hypertension, smoking, serum lipids, alcohol intake, and physical activity. Low serum DHEA was similarly predictive, confirming prior evidence that low DHEA and DHEAS are predictive of IHD.
A study by Muller et al. of aging men that examined the protective role of endogenous sex hormones in the development of atherosclerosis in aging men used measurements of carotid intima-media thickness to study endogenous sex hormones and progression of atherosclerosis.3 They found that low free testosterone levels were related to intima-media thickness of the carotid artery in older men. The association was found to be independent of cardiovascular risk factors (e.g., body mass index, waist-to-hip ratio, presence of hypertension and diabetes, smoking, etc.).
Other studies Dr. Monge found relevant included those that examined the relationship between androgen deficiency and cardiovascular as well as metabolic health, such as the study by Rosano et al.4 that found low plasma testosterone to be involved with the increased risk of coronary artery disease in male patients with angina; the Blouin et al. study,5 which investigated androgen levels in Metabolic syndrome and found significant negative correlations between androgen levels and adiposity measures, body fat distribution, and metabolic risk variables; another study by Muller et al.6 which found that higher total testosterone, bioavailable testosterone and sex hormone-binding globulin levels in aging males are independently associated with increased insulin sensitivity and reduced risk of the metabolic syndrome, independent of insulin levels and body composition measurements.
Dr. Monge also reviewed the oncology literature that has investigated the consequences of androgen deprivation therapy (ADT) on metabolic risk factors.7 Men undergoing long-term ADT experience higher prevalence of diabetes and metabolic syndrome compared with controls. Furthermore, men undergoing ADT also experience higher cardiovascular mortality, an association corroborated in a study by Tsai et al.8
Testosterone exerts several potentially beneficial effects on the cardiovascular system, Dr. Monge concluded. Low testosterone levels and androgen-deprivation therapy are associated with adverse changes in the cardiovascular risk factor profile. He echoed Dr. Jeremy Gilbert’s call for more randomized controlled trials to strengthen the evidence presented by these studies that point to testosterone’s cardioprotective effects. However, he stated that physicians can feel reassured that if a patient with metabolic and cardiovascular risk factors is in need of testosterone therapy, there is substantial evidence to allay concerns that testosterone will aggravate any cardiovascular symptoms he is experiencing and that exogenous therapy may indeed improve those symptoms.
References:
-
Zmuda JM, Cauley JA, Kriska A, et al. Longitudinal relation between endogenous testosterone and cardiovascular disease risk factors in middle-aged men. A 13-year follow-up of former Multiple Risk Factor Intervention Trial participants. American J Epidemiol 1997;146:609–17.
-
Feldman HA, Johannes CB, Araujo AB, et al. Low dehydroepiandrosterone and ischemic heart disease in middle-aged men: prospective results from the Massachusetts Male Aging Study. Am J Epidemiol 2001;153:79–89.
-
Muller M, van den Beld AW, Bots ML, et al. Endogenous sex hormones and progression of carotid atherosclerosis in elderly men. Circulation 2004;109:2074–9.
-
Rosano GM, Sheiban I, Massaro R, et al. Low testosterone levels are associated with coronary artery disease in male patients with angina. Int J Impot Res 2007;19:176–182.
-
Blouin K, Després JP, Couillard C, et al. Contribution of age and declining androgen levels to features of the metabolic syndrome in men. Metabolism 2005;54:1034–40.
-
Muller M, Grobbee DE, den Tonkelaar I, et al. Endogenous sex hormones and metabolic syndrome in aging men. J Clin Endocrinol Metab 2005;90:2618–23.
-
Shahani S, Braga-Basaria M, Basaria S. Androgen deprivation therapy in prostate cancer and metabolic risk for atherosclerosis. J Clin Endocrinol Metab 2008;93:2042–9.
-
Tsai HK, D’Amico AV, Sadetsky N, et al. Androgen deprivation therapy for localized prostate cancer and the risk of cardiovascular mortality. J Natl Cancer Inst 2007;99:1516–24.
Sponsored by an unrestricted educational grant from Solvay Pharma Inc.