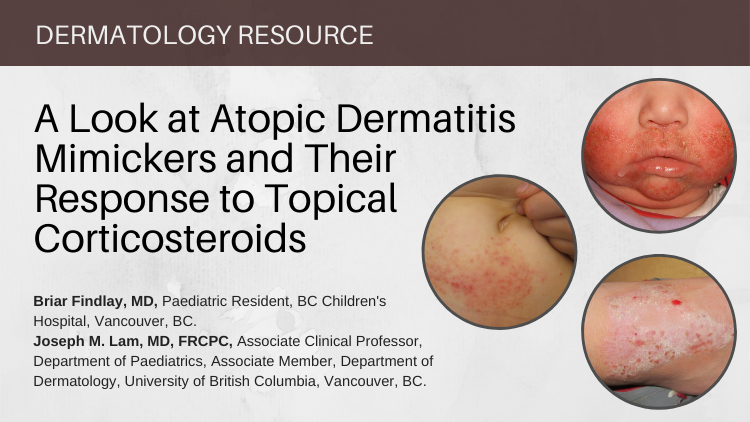
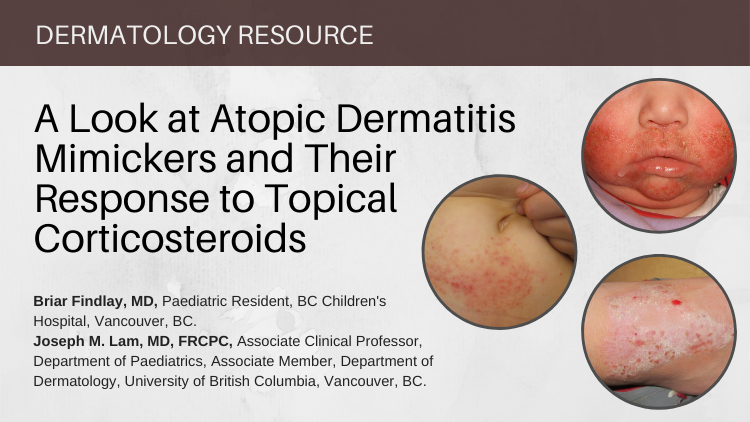
When to Scratch Beyond the Surface of the Diagnosis—A look at Atopic Dermatitis Mimickers and Their Response to Topical Corticosteroids
Members of the College of Family Physicians of Canada may claim one non-certified credit per hour for this non-certified educational program.
Mainpro+® Overview