Click here to view the entire report from the 4th Canadian Colloquium on Dementia
Idiopathic Normal Pressure Hydrocephalus
Speaker: Dr. Norman Relkin, MD, PhD, Director, Cornell Memory Disorders Program; Associate Professor of Clinical Neurology and Neuroscience, Weill Cornell Medical College; Associate Attending Neurologist, NewYork-Presbyterian Hospital, New York, NY, USA.
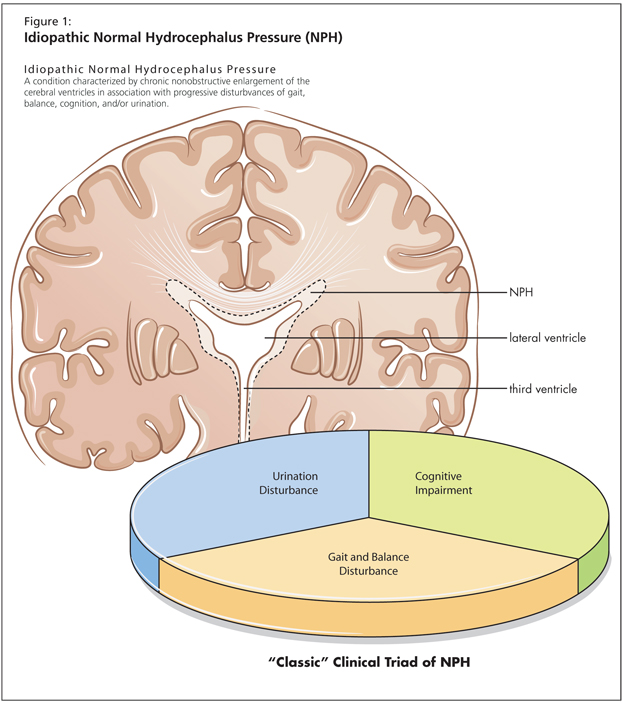
Dr. Norman Relkin discussed idiopathic normal pressure hydrocephalus (NPH), a disease commonly termed “reversible dementia.” Dr. Relkin formally defined NPH as “a condition characterized by chronic nonobstructive enlargement of the cerebral ventricles in association with progressive disturbances of gait and balance, cognition, and/or urination.” These form the so-called classic triad of NPH disturbance (Figure 1).
Dr. Relkin suggested that the triad’s shortcoming lies in its lack of universality, as the qualitative and quantitative expression of these symptoms varies. Nonetheless, the entity is often regarded as an ideal diagnosis, given these symptoms’ general applicability. Further, NPH is detectable on imaging and responds to surgical treatment with generally good long-term outcomes. However, NPH also lacks a gold standard of pathological criteria and does not respond to drug therapy (acetazolamide has been tried unsuccessfully, Dr. Relkin noted). Further, response to surgery can be inconsistent, and treatment involves a high rate of morbidity.
Diagnosing Normal Pressure Hydrocephalus
The Classic Triad
Clinical signs and symptoms, supplemented by radiologic findings, are the primary means of identifying patients with NPH. Dr. Relkin observed that researchers are working to identify biological markers for the disease in enhanced quantitative brain imaging, but integrating biomarkers into the differential diagnosis remains a future possibility.
Dr. Relkin urged his audience to be aware that the NPH-associated clinical triad is likewise not ideally reliable. One study found that, on diagnosis, ~50% of patients had the classic triad. Gait is the most reliably recognized symptom of NPH. Given that the triad is an imperfect diagnostic construct, he advised clinicians to be aware of the partial presentation of these symptoms: for example, urinary urgency is more common than frank incontinence in early stages of the disease. Overall, NPH-related disturbances may be subtle and not obviously progressive, but should be persistent.
Radiographic Evidence
Controversy lingers regarding the value of radiographic results for NPH, and, overall, there are no completely reliable quantitative measurements. The primary finding associated with NPH is atrophy. However, atrophy findings do not allow the clinician to rule out lookalike syndromes when investigating for NPH; the syndrome most commonly confused with NPH is aqueductal stenosis. Imaging characteristics of NPH include disproportionate ventriculomegaly, increased callosal angle, doming of the lateral ventricle, enlargement of the temporal horns, and expansion of the diameter of the third ventricle, often with a bowed appearance of that ventricle.
Dr. Relkin advised that cerebrospinal fluid (CSF) flow void symptoms and brain diffusivity measurements are not clear diagnostic indicators. Currently, inspection is the standard. Dr. Relkin addressed whether there is a way to distinguish the enlargement of temporal horns in NPH from that enlargement seen in Alzheimer’s disease (AD)-associated hippocampal atrophy. The hippocampus and parahippocampal folds do become more prominent in AD and can help differentiate atrophy from hydrocephalus. These areas take on a smooth, rounded contour in AD, and this can be a useful sign in some patients for distinguishing these two entities. However, Dr. Relkin advised, these can be comorbid diseases.
Features of Gait Abnormality
Gait abnormalities (incorrectly called gait apraxia) remain the best feature for recognizing NPH. Dr. Relkin advised that clinicians be alert to signs of slowed movement, decreased step height, inadequate upward angulation of the foot, diminished stride length, reduced shoulder counter-rotation relative to the pelvis, as well as increased step width and foot rotation angles. Of particular note is that patients will require 3-4 steps to perform a 180-degree turn. He emphasized that a qualitative and quantitative evaluation of gait and posture should be carried out in every case of suspected NPH.
Urinary Disturbances
Urologic evaluation may assist in differential diagnosis. Urinary disturbance, he stated, is the least consistently observed component of the NPH triad. There will be increased urinary frequency and urgency, as well as urinary incontinence (but not fecal, he noted). It is important to ask if there is nocturia, claimed Dr. Relkin. The gait disorder may impede toileting.
Cognitive Impairment
On cognitive evaluation, the hallmarks of NPH are slowed cognition, dysexecutive syndrome, visuospatial deficits, and behavioural changes. Testing may assist in assessing baseline mental status and response to treatment.
Other Signs and Symptoms Associated with Normal Pressure Hydrocephalus
Other findings indicative of NPH include increased head circumference, syncopal episodes, altered sleep architecture, and the development of systemic hypertension. The latter may occur 1-2 years prior to the onset of frank symptoms.
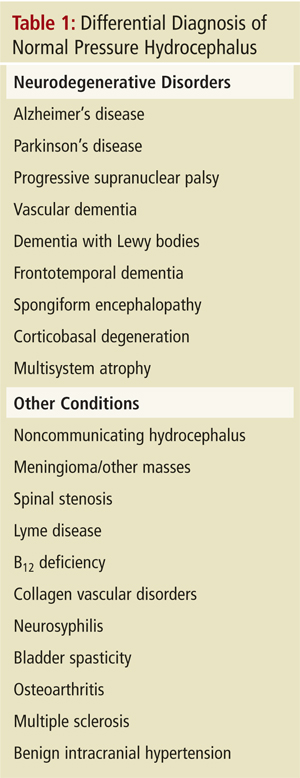
Symptoms Not Associated with Normal Pressure Hydrocephalus
Findings one would not expect in the case of NPH include papilledema, meningismus, headache, seizures (except post-shunt), or lateralized deficits. Dr. Relkin reminded listeners that the differential diagnosis is lengthy, and NPH symptoms need to be considered in light of overlapping symptomatology with lookalike syndromes (Table 1).
Given the lack of clarity around the signs associated with NPH, Dr. Relkin and colleagues worked to develop consensus criteria that were published in 2005.1 They sought to define the probably, possible, and unlikely classifications for NPH based on history, brain imaging, clinical findings and physiologic criteria. Their recommendations appear in Table 2. The criteria given do not apply to a review of shunt responsiveness.
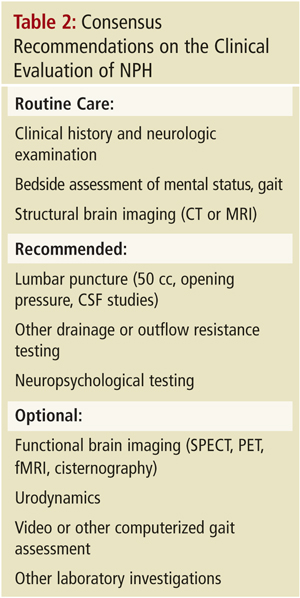
Dr. Relkin also discussed guidelines for cerebrospinal fluid drainage in the assessment of suspected NPH. The lumbar puncture tap test should involve the drawing of at least 40-50 cc’s of fluid. Gait and cognitive testing should follow within an hour of completing the tap. Continuous or intermittent draining will require hospital admission. Higher-volume drainage is more predictive of shunt responsiveness, he noted; further, a negative tap test does not preclude shunt reponsiveness.
Treatment
Programmable shunts are the new standard. They permit the opening pressure of the valve to be altered and can help to optimize treatment, but they add complication and cost. This cost is saved on the lower rates of re-operation. Complications of the shunt are the major drawback; the programmable shunt malfunction rate is 20%. Programmable shunts are part of an evolving and improving treatment process, Dr. Relkin claimed.
Conclusion
Dr. Relkin reminded listeners that NPH is one of the truly reversible causes of dementia if detected early. New technologies for diagnosis and treatment are improving disease outcomes.
Reference
- Marmarou A, Bergsneider M, Relkin N, et al. Development of guidelines for idiopathic normal-pressure hydrocephalus: introduction. Neurosurgery 2005;57(3 Suppl):S1-3.