Click here to view the entire report from the 28th Annual Scientific Meeting of the Canadian Geriatrics Society
Assessment of Fitness-to-Drive in Persons with Dementia
Speaker: Frank Molnar, MSC, MDCM, FRCP(C), Staff, Division of Geriatric Medicine, The Ottawa Hospital; Associate Professor, Department of Medicine, University of Ottawa; Affiliate Investigator, The Ottawa Health Research Institute; Scientist, The Elisabeth Bruyere Research Institute, Ottawa, ON.
Dr. Frank Molnar, a member of the network of interdisciplinary investigators for the Canadian Driving Research Initiative for Vehicular Safety in the Elderly (CanDRIVE), reviewed practical approaches to assessing fitness to drive in the setting of a dementia diagnosis.
CanDRIVE Research
The Canadian Institutes of Health Research (CIHR)-funded CanDRIVE research team has worked to produce substantive research and recommendations on fitness to drive via a two-pronged approach. First, the group has aimed at deriving and validating screening tools for this patient segment. This pillar of their work has involved building a national research team to examine medical aspects of fitness to drive in conjunction with an array of health professionals (leading to the development of tests with cut-offs based on group data), in order to pursue the second pillar of their purpose: facilitating networking and knowledge translation (leading to adjusting cut-offs and using specific findings to assess individual patients). CanDRIVE will conduct a large prospective cohort study that tracks fitness to drive among adults with dementing illness.
While the primary research is in its infancy, Dr. Molnar explained that the CanDRIVE research teams will focus on disseminating their acquired knowledge to physicians. Further, CanDRIVE aims to incorporate input from clinicians on what they should be looking at.
The Scope of the Problem
While older drivers are generally safer when compared to younger cohorts, the rate of motor vehicle crashes per km driven according to driver’s age increases beyond age 80. This shift, due primarily to the accumulation of medical illnesses in late age, means the net number of collisions and casualties will soar with an aging populace. Emergency rooms will treat an increasing number of older crash victims.
Projections through 2026 from Transport Canada show that crashes will rise primarily in older groups. An older person involved in a crash has a fourfold higher likelihood of being seriously injured or hospitalized; has a higher risk of becoming permanently disabled or dying; and takes longer to recover. Studies have shown that the majority of crash-injured seniors were driving the vehicle, and that most of the crashes involving older drivers are multivehicle and involve innocents. Dr. Molnar asked listeners to consider that they are not doing older drivers a favour by letting them drive when they reach the limit of their ability to do so safely.
The Problem Is not Age Alone
The vast majority of older drivers are safe drivers, Dr. Molnar insisted, and CanDRIVE is sensitive to the concern that their work contributes to ageism or alarmism about seniors at the wheel. He emphasized that medical conditions and medications are the primary cause of older drivers’ incompetence, and any medication can contribute to collision risk. Older people are affected disproportionately due to polypharmacy.
Dr. Molnar explicitly stated that no disease or chronic condition can be isolated as categorically risky. It is not the presence but severity and/or instability of conditions, plus high doses and/or changing doses of medications, that are perilous. While physicians cannot prevent every accident, they are well-placed to detect many persons who are at risk for unsafe driving. Qualities of medical conditions or medications most correlated with impaired driving capacity are those that alter physical, sensory, mental, or emotional abilities.
Driving recruits a complex set of cognitive capacities and behaviours, including operational, tactical, and strategic categories of action. Doctors cannot correctly assess impaired function 100% due to limitations of the physical exam (which is primarily designed to detect presence or absence of disease, not to assess function or safety) and the inadequate time available in front-line clinical settings. For example, tactical maneuvering is involved in decisions drivers make on the road—it supports real-time contextual decisions. Impairments in this category are often hard for doctors to catch. Strategic capacity refers to decisions made before getting on the road, which is difficult for doctors to assess. No screening tool will ever be completely effective for screening for all motor vehicle crashes. Most assessment protocols only test stable intrinsic features of driving ability. Doctors may miss new or fluctuating illness. Further, physicians cannot anticipate patients’ judgment of extrinsic factors such as weather, other drivers, road conditions, or a car’s safety.
Clinical Assessment: An Overview of the Issues
Assessment can be improved, however CanDRIVE seeks to galvanize attention on this issue as it is well-documented that cognitive impairment puts drivers at increased risk of at-fault crashes. A 2004 study found that currently there are tens of thousands of older drivers with dementing illnesses in Ontario; by 2028, the figure will approach 100,000.
A diagnosis of dementia does not automatically mean no driving, Dr. Molnar stated; however, a diagnosis of dementia means that the clinician must ask if the person is still driving, and driving safety must be assessed and documented. Provincial reporting requirements vary but uniformly state that the condition must be assessed and reported.
The Canadian Medical Association’s (CMA) guidelines, “Determining Medical Fitness to Operate Motor Vehicles” (7th ed.), joins international consensus statements that recognize the limitations of available data on assessment but recommend that: one, those with moderate to severe dementia should not drive (CMA: Moderate = 1 ADL or 2 IADLs impaired due to cognition); two, that individual assessment should be performed for those with mild dementia; three, that periodic follow-up is required (every 6-9 months); and four, the “gold standard” is comprehensive on-road assessment. Dr. Molnar opined that the CMA guidelines should go further in terms of ADLs—any single IADL impairment due to cognition should trigger an assessment of fitness to drive. Further, he finds the 6-9 month follow-up rule insensitive and advises an individualized approach (e.g., assessing every 3 months in the setting of rapidly progressing disease).
Dr. Molnar cautioned that while clear assessment protocols are given (e.g., for using the MMSE, Clock Drawing, Trails B), no guidance is provided as to how physicians should apply such tests. For example, how to respond to different scores, what cut-offs to use, and which errors equal automatic failure remain under debate. CanDRIVE has examined dozens of dementia and driving articles, and was unable to find one cognitive test that was analyzed via a validated cut-off. Clinicians are working in an evidence-based vacuum, Dr. Molnar stated.
An Approach to Assessing Fitness to Drive
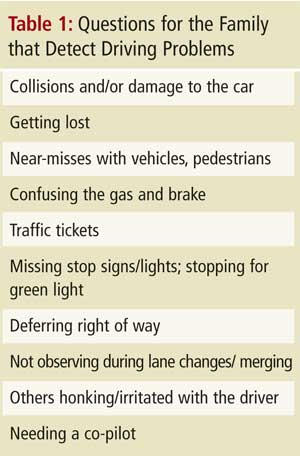
Clinicians must inquire, “Do you drive?” Failure to verify has not protected clinicians in litigation, Dr. Molnar advised. Two, recall that driving capacity depends on a global clinical picture, including the patient’s cognition, function, physical abilities, medical conditions, behaviour, and driving record. Then, follow general questions with specific cognitive tests. Corroborative information from the family can help, and Dr. Molnar suggested several areas of inquiry that are best asked when the patient is not in the room (Table 1). Further, review medical conditions that when severe, poorly controlled, or changing rapidly can compromise capacity to drive (he suggested clinicians ask themselves, “Would I get in a car with this person based on these findings?”). Dr. Molnar recommended that the “3 Ds”— dementia, delirium, and depression— are most important to consider. He then reviewed medications that could affect driving (Table 2).

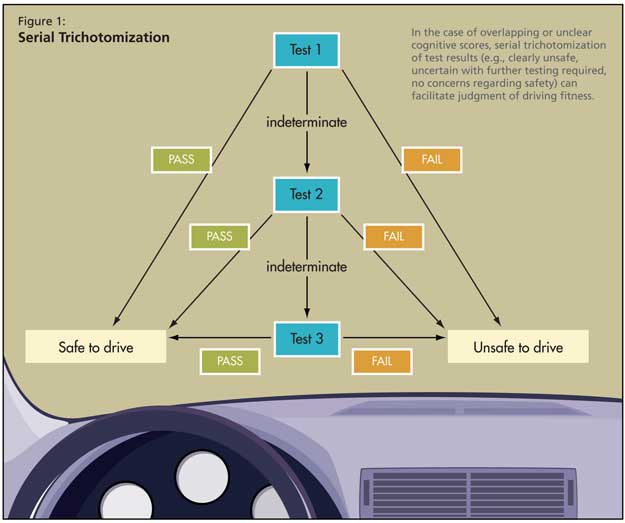
The key intervention is to test specific cognitive domains, as with the aforementioned protocols. Judgment is assessed by the test response to dangerous situations (e.g., fire); visuospatial ability is tested with the MMSE and clock drawing; executive function is assessed with Trails A and B, clock drawing, and 1-minute animal naming; and reaction time can be verified with the ruler drop test. In the case of overlapping/unclear cognitive scores, he argued for serial trichotomization (e.g., clearly unsafe, uncertain with further testing required, no concerns regarding safety), as shown in Figure 1.
He advised that the MMSE is the best place to start; patients scoring under 20 are likely unsafe to drive. All areas of testing mentioned yield valuable data; the ruler drop test, while not validated, is important in assessing reaction. Such tests are valuable because decrements of reaction time (which is not tested in the physical examination) often only become apparent outside of testing when lapses involve seconds. However, driving involves the need for reactions on a millisecond scale.
Conclusion
Dr. Molnar closed with emphasizing that if dementia is diagnosed, driving must be asked about, formally assessed, and documented. Physicians can perform a comprehensive driving safety clinical evaluation in approximately 15 to 20 minutes. If clinicians are unsure of safety, refer to specialized assessment or specialized on-road testing. In dementia, reassess driving safety every 6 to 9 months. Finally, he encouraged those with any ideas about driving assessment to bring them to the attention of CanDRIVE staff via their website (www.candrive.ca).