L’apathie dans la démence est un important défi comportemental
Conférencière : Tiffany Chow, M.D., Clinicienne-chercheure, Institut de recherche Rotman ; Professeure adjointe, Neurologie et psychiatrie gériatrique, Université de Toronto, Toronto, ON.
La Dre Tiffany Chow a commencé par exprimer toute son estime, en tant que neurologue, à l’égard de ses collègues en gériatrie, dont elle admire la défense d’une approche plus holiste des patients atteints de démence, et de l’importance du travail d’équipe.
Elle a défini des aspects fondamentaux de la qualité de vie des personnes atteintes de démence : ne pas avoir de douleurs ; se sentir en sécurité ; pouvoir participer à des activités intéressantes ; et être à même de conserver le plus haut degré possible d’autonomie. La Dre Chow a également décrit des facteurs de qualité de vie pour les aidants : des liens affectifs ; la capacité d’aider le patient (p. ex., en le nourrissant) ; passer de bons moments ensemble ; et savoir que tout ce qui peut être fait est fait.
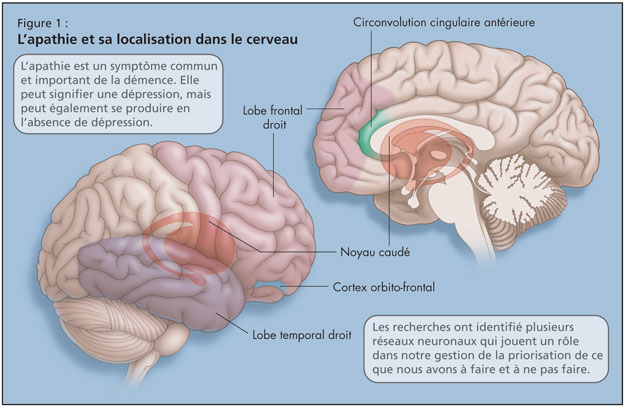
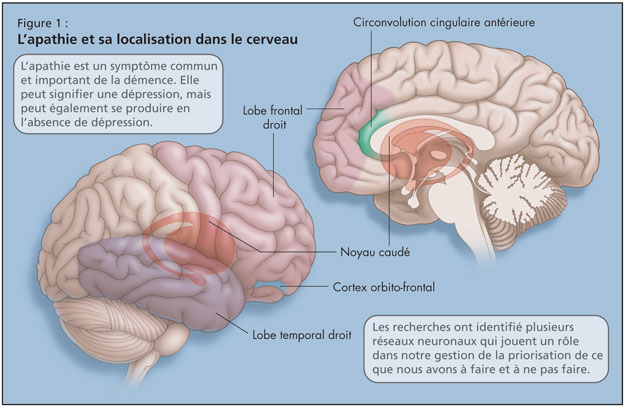
La Dre Chow a mis en garde contre les effets de l’apathie chez les patients atteints de démence, qui peut avoir des répercussions sur toutes les dimensions de la qualité de vie décrites précédemment. L’apathie est un symptôme commun et important de la démence. Bien que l’apathie puisse signifier une dépression, elle peut aussi survenir en l’absence de dépression, et chacune peut exacerber l’autre. L’apathie peut empêcher les patients atteints de démence d’être motivés à prendre physiquement part à des activités quotidiennes et, du fait du manque de stimulation, cet état peut hâter le déclin cognitif.1 L’apathie intensifie aussi le désarroi de l’aidant, et nuit au lien affectif avec le patient. Elle diminue également l’adhésion au traitement (pharmacologique ou autre, p. ex. ludothérapie). L’apathie peut contribuer au placement en établissement ; des études ont révélé des taux plus bas d’apathie parmi les patients résidant dans leur communauté.
La Dre Chow a expliqué qu’il existe plusieurs réseaux neuronaux qui gèrent notre façon de prioriser ce que nous avons à faire et à ne pas faire, et une tentative de localiser l’apathie dans le cerveau a été faite (Figure 1). La recherche sur l’apathie a mis en évidence son lien avec le lobe temporal droit, le lobe frontal droit, le noyau caudé, la circonvolution cingulaire antérieure (ou le cortex frontal médian supérieur), et le cortex orbito-frontal.2
Dans leur étude récente,3 la Dre Chow et ses collègues ont cherché à déterminer de façon empirique des groupements de symptômes d’empathie, chez des patients atteints de démence, pour voir si les symptômes affectifs, comportementaux ou cognitifs de l’apathie avaient tendance à se produire ensemble ou de façon isolée, et si l’apathie se ma-nifestait typiquement en cooccurrence avec d’autres types de désordres comportementaux.
La Dre Chow a montré des données provenant de Baycrest, Sunnybrook [Centre des Sciences de la Santé], UC San Francisco, et UCLA, combinées pour donner les résultats de l’Inventaire neuropsychiatrique (NPI). Dans la section du NPI traitant de l’apathie, des patients sont interrogés sur l’activité spontanée, la spontanéité conversationnelle, la participation à leurs anciennes activités et à d’anciennes tâches, la démonstration de leur intérêt pour autrui, leur relations avec leurs amis et leur famille, et le degré d’affection.
Les résultats ont montré que, chez ceux qui présentaient soit une DFT, soit une démence de type Alzheimer (DTA), le type d’apathie le plus courant était, le cas échéant, une diminution de l’activité spontanée. Une comparaison du pourcentage d’apathie dans les deux types de démence a montré qu’il y avait plus de patients atteints de DFT (72 %) qui présentaient aussi une apathie que ceux qui avaient une DTA (56 %).
Ils ont également fait apparaître tous les types d’apathie : apathie affective (émoussement émotionnel) ; apathie comportementale (manque d’activation spontanée) ; et apathie cognitive (manque d’intérêt à s’engager dans une nouvelle activité cognitive). De nombreux patients présentaient les trois types, et presque tous en présentaient au moins deux. Et c’était le cas pour les deux types de démence.
Ils ont recherché sur le NPI une association entre l’apathie et d’autres variables non liées à l’apathie, comme l’impulsivité, l’angoisse de séparation et le comportement de résistance, et ont trouvé que ceux qui présentaient une apathie de type affectif étaient plus susceptibles d’avoir ces symptômes que ceux présentant d’autres types d’apathie ou aucune apathie.
Elle a parlé des résultats d’une étude de Robert et coll.4 qui indiquent que l’apathie peut être un prédicteur, en vertu duquel des patients ayant un trouble cognitif léger (TCL) évoluent en DTA.
Deux groupes, l’un en Amérique du Nord, l’autre en Europe, travaillent à faire inscrire l’apathie au DSM-V (Manuel diagnostique et statistique des troubles mentaux). Les critères en seraient le manque de motivation (relativement aux conditions initiales), le manque d’acti-vités dirigées vers un but (apathie cognitive), le manque d’intérêts ou de buts, et des réponses émotionnelles affaiblies (émoussement émotionnel).
Il convient d’envisager le traitement de l’apathie selon le type d’apathie.1,5 Pour ceux qui présentent une apathie affective, un antidépresseur pourrait être de rigueur. On peut utiliser les psycho-stimulants dans l’apathie comportementale. Les inhibiteurs de la cholinestérase ont démontré une efficacité sur l’apathie cognitive. On a montré l’efficacité et la bonne tolérance de psychostimulants comme le méthylphénidate ; bien que la dextroamphétamine appartienne à la même classe thérapeutique, on ne dispose de preuves suffisantes que pour l’usage du premier. Des antidépresseurs et des agents dopaminergiques ont également été utilisés.
La Dre Chow a examiné si certains de ces médicaments, comme les neuroleptiques ou d’autres calmants, pouvaient occasionner une apathie en cas de démence. Avec ses collègues, elle a examiné ce point au cours d’une étude transversale chez 69 patients atteints de DFT. Sur les quatre médicaments de ce groupe les plus couramment utilisés – les anti-inflammatoires non stéroïdiens (probablement contre les symptômes de douleurs arthritiques), les inhibiteurs sélectifs du recaptage de la sérotonine, les inhibiteurs de la cholinestérase et les neuroleptiques – elle n’en a trouvé aucun qui augmente le risque d’apathie.
La Dre Chow a recommandé les articles de Robert et coll., 20096 et de van Reekum et coll., 20051 à ceux qui désirent en apprendre d’avantage sur l’apathie.
Références:
-
van Reekum R, Stuss DT, and Ostrander L. Apathy: why care? J Neuropsychiatry Clin Neurosci 2005;17:7–19.
-
Mendez J, Lauterbach EC, and Sampson, SM. An evidence-based review of the psychopathology of frontotemporal dementia: a report of the ANPA Committee on Research. J Neuropsychiatry Clin Neurosci 2008;20:130–49.
-
Chow TW, Binns MA, Cummings JL, et al. Apathy symptom profile and behavioural associations in frontotemporal dementia vs. Alzheimer’s disease. Arch Neurol 2009;In press.
-
Robert PH, Berr C, Volteau M, et al. Importance of lack of interest in patients with mild cognitive impairment. Am J Geri Psych 2008;16:770–6.
-
Malloy PF and Boyle PA. Apathy and its treatment in Alzheimer’s disease and other dementias. Psychiatric Times 2005;XXII(13).
-
Robert P, Onyike CU, Leentjens AF, et al. Proposed diagnostic criteria for apathy in Alzheimer’s disease and other neuropsychiatric disorders. European Psychiatry 2009;24:98–104.