Things that fascinate me about radiology
I was a family physician for 7 years before becoming a radiologist. There are some things I miss about family practice. I miss the longitudinal relationship that I often had with multiple generations of family members.
There are also some things that fascinate me about radiology. For instance, improving computer and imaging technology has translated into imaging developments that can be used to benefit patients. Just a few years ago, we wouldn’t have thought we could adequately screen the colon for colon cancer and pre-cancerous lesions such as polyps. Now, in patients who cannot have a colonoscopy, we routinely perform CT colonoscopy (CTC), giving an alternative means of screening and diagnosis in these patients.
An article in the New England Journal of Medicine suggests that CTC could be used for primary screening, however, we mainly use it for patients who have failed colonoscopy – often because of a redundant sigmoid colon which cannot be navigated by the scope. We can even do the study the same day, as the patient has already undergone a bowel preparation. We do give them contrast to tag any residual fluid and stool in the colon to be able to differentiate it from colonic pathology.
We perform CT prone and supine to allow us to exam all the walls of the colon without any overlying fluid. Then we use computer software to generate 3 dimensional images of the colon that we can “fly through” to assess for mucosal lesions. Of course, the CT images are also examined for any extra- mucosal findings. I have diagnosed an unsuspected renal cell carcinoma on a patient being screened for colon cancer.
Below is a picture from my practice. It shows the colon distended with carbon dioxide – we use a small rectal tube and a regulated pump to inflate the colon. The technique readily shows the “napkin-ring” constricting lesion in the cecum. The 3D images show the lesion as it would be seen by the scope!
I would love to hear how imaging has affected your practice, both positive and negative.
Reference:
CT Colonography versus Colonoscopy for the Detection of Advanced Neoplasia
David H. Kim, M.D., Perry J. Pickhardt, M.D., Andrew J. Taylor, M.D., Winifred K. Leung, M.D., Thomas C. Winter, M.D., J. Louis Hinshaw, M.D., Deepak V. Gopal, M.D., Mark Reichelderfer, M.D., Richard H. Hsu, M.D., and Patrick R. Pfau, M.D.
N Engl J Med 2007; 357:1403-1412; October 4, 2007
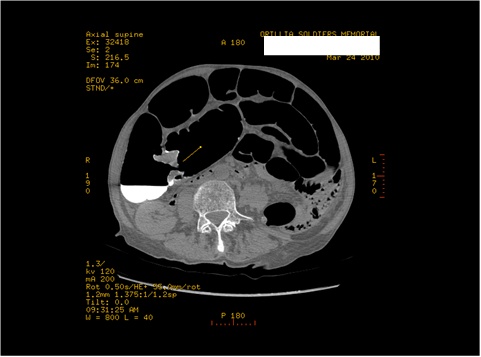
Axial view with the “Napkin-ring” mass seen in the region of the cecum-ascending colon.

Coronal Image showing the lesion.
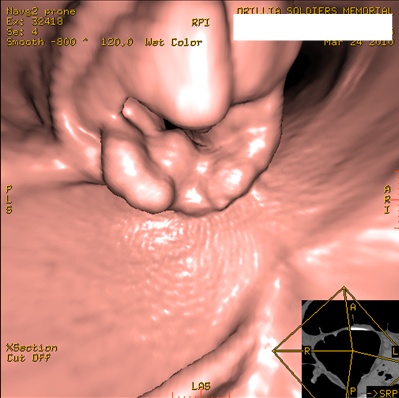
3D image showing the lesion almost identical to how it would appear on Colonoscopy, had this patient been able to have colonoscopy.
